Health Literacy: What It Is and How to Improve It
What Is Health Literacy?
Health literacy is the ability to access, understand, and act on information that affects one’s health. While literacy refers to the ability to read and write, health literacy is more complex. Many internal and external factors are at play, for instance, a person’s math skills and a healthcare provider’s cultural background. And while literacy informs a person’s ability to be successful in school or at work, health literacy can have life-or-death consequences.
In addition, the economic toll of poor health literacy is between $108 and $328 billion per year. To put this in perspective, the potential savings of improved health literacy matches the cost of providing healthcare coverage to the nearly 50 million Americans who were uninsured in 2006 (based on U.S. Census Bureau estimates). When the future implications of poor health literacy are considered, this cost is predicted to compound to between $1.6 and $3.6 trillion.
Why Health Literacy Is Important
Well-informed patients naturally feel more confident interacting with healthcare professionals and making medical decisions. Studies also suggest that patients with poor health literacy have worse medical outcomes. Broadly speaking, poor health literacy impacts adherence and compliance to medication. In clinical trials, poor health literacy impacts recruitment and retention.
Poor health literacy is also associated with decreased preventive care and increased use of emergency medical services, which are not only more costly to the patient and the healthcare system as a whole, but also reduce a patient’s chances of positive treatment outcomes due to delayed intervention. For instance, if a patient puts off seeing his/her doctor for a cough that turns out to be lung cancer, the prognosis is likely to be worse, and treatment options more limited, than a patient who had visited his/her doctor soon after symptoms arose.
Put simply, proficient health literacy puts the patient in the driver’s seat, resulting in more consistent, compliant, and effective healthcare for the patient—and also one that is more cost-efficient.
Factors that Affect Health Literacy
Health literacy depends on a complex matrix of factors, including:
- General communication skills
- Cognitive abilities
- Learning abilities
- Educational opportunities
- Culture
- Cultural beliefs
- Values
- Traditions
- Attitudes toward medicine
- Language
- Written literacy
- Digital literacy
- Visual literacy
- Computational literacy
Depending on the situation (e.g., the patient/healthcare provider’s relationship or the environment), different combinations of these factors can come into play. For instance, a patient who shares the same cultural background as his/her healthcare provider may feel more comfortable and have an easier time communicating because they share not only the same language or dialect but also hold the same cultural beliefs and values.
5 Ways to Improve Health Literacy
Because health literacy is a systemic problem, the onus of improving it does not fall on the patient. Healthcare providers and institutions must work to better educate patients, meet them on their level, and ensure medical options, instructions, and treatment plans are fully understood. The following are some of the ways healthcare providers can improve the health literacy of their patients and their caregivers.
1. Improve Patient Educational Materials
Patient education is a collective term for the process in which doctors, nurses, and other healthcare professionals pass on information to their patients and their families or caregivers. The effectiveness of this process can have long-term impacts on patients’ health, both positive and negative.
Today, this information transfer can take place in a variety of ways—from the traditional pamphlets you see in waiting rooms to podcasts, videos, and even comic books. Whatever the method, the most important thing for healthcare professionals to remember when selecting resources for their patients is to meet them on their level. For instance, educational materials for children should be engaging, relatable, and visually compelling. When patients are able to connect with educational materials in a more meaningful way, they are better able to receive and retain the often complicated information being imparted to them.
Check out Jumo Health’s collection of age-appropriate educational materials.
2. Provide Regular Staff Education
To improve patient education, and consequently health literacy, medical staff must be trained in best practices for delivering educational material. Therefore, all staff should receive regular, standardized training on how to best educate patients.
3. Use Plain Language When Communicating With Patients
Plain language refers to communication that can be understood by the recipient the first time it’s presented. Using plain language is one way healthcare providers can help improve health literacy. By using clear terminology, patients have a much better chance of understanding their condition, options, treatment plan, and doctor’s instructions. Plain language can also help break down other potential barriers to communication, like the sense of inferiority that comes with feeling like you’re being talked down to. This is true of both conversational and written communication.
It’s also important to note that what is considered to be plain language to one person may not be to another. For this reason, testing your plain language communication with patients can help determine where gaps may still exist and where adjustments may need to be made (on a person-by-person or community basis).
When used effectively, plain language can go a long way toward satisfying the main components of health literacy: enabling the patient to better access, understand, and act on the (often) complicated information being presented to them. Some of the ways healthcare providers can incorporate plain language practices into their communication include:
- Using active voice as much as possible
- Using a hierarchical approach (starting with the most important information)
- Avoiding jargon
- Taking time to break down complicated topics and terminology
Along with using plain language as a best practice, healthcare providers should also be sure to clearly spell out the basics: what, why, when, and how. For instance, when antibiotics are prescribed, it’s important that a healthcare provider explains the purpose of the drug and how it will affect the patient’s condition, why it must be taken twice per day for the duration of the prescription (and the consequences of not doing so), and how it should be taken with food to prevent nausea. It can be easy for healthcare providers to gloss over these seemingly small, but important details after having prescribed the same medication hundreds of times over the years.
4. Demonstrate Cultural Competency
Because culture plays a large role in how people communicate, healthcare providers must pay special attention to how they transmit information to patients with different cultural backgrounds. As mentioned above, differences in a patient and their healthcare provider’s cultural beliefs, values, traditions, and attitudes toward medicine—and, of course, language—can all be barriers to effective communication.
When healthcare providers address patients of different cultural backgrounds in a respectful and culturally relevant manner, there is a much better chance the patient will hear and retain the crucial information being conveyed. In addition to being conscientious of how patients are addressed, there are many resources available to healthcare providers who want to become more culturally competent. This investment can make a noticeable difference in treatment outcomes.
In terms of language, the National Standards for Culturally and Linguistically Appropriate Services in Health Care recommends that healthcare providers offer language assistance services at no cost to the patient. In fact, most states (as well as Title VI of the Civil Rights Act of 1964) now require this. While it’s ideal for medical offices to have bilingual employees on staff, translation services and interpreters can also help bridge communication gaps for patients with limited English proficiency. The standards report also advocates for having educational and print materials available in languages that are common to regional populations.
5. Request Patient Feedback
Despite healthcare professionals’ sound intentions of accurately communicating medical information, the intricacies of the message can easily be lost in translation. For instance, a patient with proficient health literacy skills receiving a life-changing diagnosis from their doctor may not fully process the conversation or retain some of the more crucial details. The emotional impact of the diagnosis may temporarily affect the patient’s ability to process information, and some important details of the condition may not be received and understood as intended.
This is where feedback comes in. Soliciting patient feedback is a solid way of not only assessing health literacy but also ensuring the information given matches the information received by the patient. This feedback could come through a variety of methods, which should be used in tandem for best results, including:
- Asking a patient to repeat information back to you (also referred to as the “teach-back” method)
- Allowing time for questions and answers at the end of an office visit
- Following up with a phone call after a visit
- Administering patient experience surveys
Low Health Literacy: Who is at Risk?
While there is a correlation between literacy and health literacy, no one is immune from health literacy challenges. Only 12% of American adults are considered proficient in health literacy and more than a third have only “basic” or “below basic” health literacy levels. This equates to nearly 80 million Americans who have trouble following simple medical instructions provided by their medical professional or making the appropriate determinations on whether treatment should be sought, for example.
The following are some of the populations most at risk of health literacy challenges:
- Older adults
- Minority populations
- Uninsured populations
- Low-income populations
- Populations with limited education
- Populations with limited or no English proficiency
- Immigrant and refugee populations
Older Adults
Adults 65 years of age or older have been shown to have lower health literacy levels than those under 65. This disparity is most striking for the 75-and-over group, with more than two-thirds of adults showing basic or below basic health literacy skills.
Minority Populations
While adults in any racial and ethnic group can have basic or below basic health literacy, white/Caucasion adults represent the smallest portion (28%) in these categories. By contrast, 66% of Hispanic adults have basic or below basic health literacy skills, and black/African-American adults have 57%. When the below basic category is considered on its own, 41% of white/Caucasion adults and 35% of Hispanic adults make up this designation.
Uninsured Populations
The uninsured and those with Medicaid or Medicare are four times more likely to have below basic health literacy skills than those with employer-provided insurance. For those with employer-provided insurance, the proportion of adults with basic or below basic health literacy is approximately one-fourth, whereas more than half of the uninsured population and those with Medicaid or Medicare make up these groups.
Low-Income Populations
Lower incomes are also associated with poor health literacy. Those living below, at, or just above the poverty level have an average health literacy in the basic range, compared to intermediate (just below proficient) for those whose income is at least 175% of the poverty level.
Populations with Limited Education
Education and health literacy are closely linked. For instance, only 1% of those with less than a high school education are considered proficient in health literacy, compared to 30% of those with a bachelor’s degree. The story is even more telling for the group with below basic health literacy; 49% of those with less than a high school degree and just 3% of those with a college degree fall into this category.
Populations with Limited or No English Proficiency
Because English proficiency is a prerequisite for health literacy in America, populations with limited or no English language skills are at increased risk of having poor health literacy.
Immigrant and Refugee Populations
The American healthcare system is complex and can be difficult to navigate for those who were born here, let alone those who were not. For immigrants and refugees coming from other countries with entirely different healthcare services, practices, and insurance systems, it can be overwhelmingly complicated.
Understanding Hemophilia For All Ages
Jumo Health and the National Hemophilia Foundation seek to increase health literacy with the release of four evidence-based comic books for those managing hemophilia
NEW YORK, NY (March 2019) – Global health education company Jumo Health is releasing four new comic books that provide contextual and age-appropriate information for children, teenagers, and families managing hemophilia, a bleeding disorder.
The books, created in collaboration with the National Hemophilia Foundation (NHF), break down a variety of topics, including what clotting factors are and how to successfully manage the condition on a daily basis. As with all Jumo Health titles, the books are evidence-based, peer reviewed by leading physician specialists, and based on real patient stories to ensure authenticity.
“At NHF we recognize the need for people with bleeding disorders to be educated about their condition in age-appropriate ways. These books demystify the science behind bleeding disorders while acknowledging the emotional component of living with a chronic illness,” stated Kate Nammacher, Senior Director of Education at the National Hemophilia Foundation.
Each of the four comic books targets a different age cohort including a toddler, adolescent, teenager, and adult caregivers as they navigate through the diagnosis of, and subsequently living with, hemophilia. The books are written in a complementary style appropriate to each target age group, making this collection of books a comprehensive resource for those affected by hemophilia.
“For decades we’ve watched as statistics surrounding reading comprehension, health literacy, and medication compliance remain fundamentally unchanged,” shared Kevin Aniskovich, President and Chief Executive Officer of Jumo Health. “With only 20% of patients receiving information when initially diagnosed, it’s no surprise that many patients don’t have the tools to succeed. We are delighted to work with NHF to reverse this trend and to ensure these resources get into the hands of patients, caregivers, and health care professionals.”
The importance of having age-appropriate resources such as these is echoed by Jason, whose family and son Ben are featured in Understanding Hemophilia for Families. “Sharing through an easy read -like a comic book- is perfect; it ties a real story into what would otherwise be a complicated disorder to understand. We are honored to have been asked to share our story and Ben’s walk with hemophilia.”
Families can email NHF’s HANDI directly for individual requests. The books are also available for purchase online at the Jumo Health store.
About The National Hemophilia Foundation
The National Hemophilia Foundation (NHF) is dedicated to finding better treatments and cures for inheritable bleeding disorders and to preventing the complications of these disorders through education, advocacy and research. Established in 1948, the National Hemophilia Foundation has chapters throughout the country. Its programs and initiatives are made possible through the generosity of individuals, corporations and foundations as well as through a cooperative agreement with the Centers for Disease Control and Prevention.
Visit the National Hemophilia Foundation.
Jumo Health Named as Finalist for the Inaugural Sharecare Awards
Two Videos from the Global Health Education Provider Make the Cut
NEW YORK, NY (January 20, 2019) – Jumo Health, a global provider of age appropriate health education, is proud to announce that it has been recognized as a finalist for the inaugural Sharecare Awards, a competition to inspire and honor the creators of health and wellness broadcast and digital media programming. The Sharecare Awards is in association with The National Academy of Television Arts & Sciences, New York Chapter, which fosters creativity and inspires artistic and technical excellence through the renowned Emmy® Award.
“Our finalists represent some of the highest impact and most innovative and creative work in health media, and we are calling on the public to help us celebrate these achievements,” said Dawn Whaley, president of Sharecare.
Jumo Health Honored for Two Videos
The first, a mixed media video using live action and computer generated imagery, “An Inside Look at MPS I,” developed in partnership with Sanofi Genzyme, combines a real patient’s story with CGI animation to dive inside the body of this rare disease.
The second video to be selected explores Familial Hypercholesterolemia using 2D animation and storytelling to educate on complexities of the disease in a format and style the entire family can understand.
“Baked into the DNA of our Company, is the desire to remove the fear and anxiety that often accompany a clinical diagnosis,” shared Kevin Aniskovich, chief executive of Jumo Health. “Our work with patients and the broader advocacy community allows us to create authentic, relevant, and actionable materials that increase health literacy to ensure long term adherence for our clients. To have our work and people recognized for our commitment to the community is truly humbling,” concluded Aniskovich.
The winners will be announced on March 14, 2019 at special event in Atlanta. Voting is open to the public now through January 25, 2019 on https://sharecareawards.org/voting/.
Sharecare Names Finalists for Inaugural Sharecare Awards
Public voting open for Sharing Care Award until Jan. 25; all Sharecare Award winners revealed on March 14 at special event in Atlanta and via Facebook Live
ATLANTA (January 16, 2019) – Sharecare, the digital health company that helps people manage all their health in one place, today announced the finalists in the Sharecare Awards[i], a competition to inspire and honor the creators of health and wellness broadcast and digital media programming that demonstrate “sharing care.” The Sharecare Awards is in association with The National Academy of Television Arts & Sciences, New York Chapter, which fosters creativity and inspires artistic and technical excellence through the renowned Emmy® Award.
“Our finalists represent some of the highest impact and most innovative and creative work in health media, and we are calling on the public to help us celebrate these achievements,” said Dawn Whaley, president of Sharecare. “By recognizing such exemplary work, we hope to inspire others not only to continue driving awareness and important discussions around wellbeing issues, but also to take an active role in making themselves and their communities healthier.”
Each finalist also is eligible to win the Sharing Care Award, a special award bestowed to the entrant that receives the most votes from the general public between now and Friday, Jan. 25, 2019, at www.sharecareawards.org/voting. The inaugural Sharecare Awards will culminate on Thursday, March 14, 2019, with a special event in Atlanta that will be streamed via Facebook Live. In addition to honoring finalists and announcing winners for each category and the Sharing Care Award, three additional awards – two Humanitarian Awards, one to an individual and the other to an organization, and a Lifetime Achievement Award – will be presented at the event.
Selected by the Sharecare Awards Academy of Judges, a panel of 23 renowned experts in health and media, the category finalists for the inaugural Sharecare Awards are:
Behavioral Health
- “A Doctor’s Struggle with Opioid Addiction,” Nobody Told Me!
- “Family 60 on Schizophrenia,” Ipromise2
- “Finding Help for Opioid Addiction,” The Wellness Network
- “Ipromise2 Mental Health Awareness Campaign,” Ipromise2
- “MedCircle Original Series on Depression featuring Dr. Sue Varma,” Dr. Sue Varma & the MedCircle Team
- “Pip,” Southeastern Guide Dogs
Caregiving/End of Life
- “Caregiver Self-Care: Physical Activity,” American Cancer Society
- “Choose to Prepare,” Betty Irene Moore School of Nursing at the University of California, Davis
- “Defining Hope,” Carolyn Jones Productions
- “Kim & Dustin,” AARP
- “Strategies to be a Successful Caregiver,” The Wellness Network
Chronic Conditions
- “An Inside Look at MPS I,” Jumo Health
- “Love is Patient,” Carcinoid Cancer Foundation
- “Taking Control of Your Diabetes,” TCOYD
- “The Gift of Life,” Carcinoid Cancer Foundation
- “This Is Living With Cancer,” Pfizer
- “Understanding Familial Hypercholesterolemia,” Jumo Health
Health/Science: News
- “Aids,” WPIX-TV
- “Diabetic Sticker Shock,” WTEN
- “Fingernails Can Detect Signs of Serious Illness,” WPIX-TV
Health/Science: Program/Special
- “Childhelp Merv Griffin Village,” Childhelp
- “Freedom from Fibroids,” Atlanta Fibroid Center
- “The Gift of Mobility,” Women Orthopaedist Global Outreach
- “The Healing America Campaign: Chapter One,” PlantPure Productions, LLC
Healthy Living
- “A Fairy Tale Ending,” American Heart Association
- “Angelica Hale, Heart Your Kidneys PSA,” National Kidney Foundation
- “Healthy Living Video Shorts,” American Heart Association
- “HealthyWomen.org,” HealthyWomen
- “How to Eat & Sleep Your Way to Being Younger & ‘AgeProof,’” Michael F. Roizen MD, Cleveland Clinic Wellness
- “KidsHealth.org,” Nemours
- “Life’s Simple Seven,” American Heart Association
Innovation
- “Doctor Mike YouTube,” Doctor Mike
- “First-Ever Micro-Laparoscopic Hysterectomy,” Dignity Health Saint Francis Memorial Hospital
- “Google Fit ‘Heart Points’ and American Heart Association,” American Heart Association
- “Gripbell,” Flip2Media, Inc.
- “Innovative Therapy in Zero Gravity,” Diveheart
Public & Community Health/Policy
- “Angelica Hale for THE BIG ASK: THE BIG GIVE PSA,” National Kidney Foundation
- “Defining Hope,” Carolyn Jones Productions
- “Tomodachi J&J Disaster Nursing Training Program,” Johnson & Johnson
- “Tracy and Dr. Scantlebury PSA,” National Kidney Foundation
Sexuality/Gender Identity
- “Jack’s Caregiving Coalition,” AARP
- “Kim & Dustin,” AARP
- “Male Caregivers in Philadelphia,” AARP
- “The Rainbow Has a Silver Lining: LGBTQ Aging Issues,” Lifestyle Home Solutions
More information about the Sharecare Awards is available at https://sharecareawards.org.
About The National Academy of Television Arts and Sciences, New York Chapter
The National Academy of Television Arts and Sciences, New York Chapter, founded in 1955, is the preeminent membership organization serving media professionals by offering career enhancing events and networking opportunities. New York NATAS fosters creativity and inspires artistic and technical excellence through the renowned Emmy® Award, the coveted peer-recognition symbol of distinction in regional television.
About Sharecare
Sharecare is the digital health company that helps people manage all their health in one place. The Sharecare platform provides each person – no matter where they are in their health journey – with a comprehensive and personalized health profile where they can dynamically and easily connect to the information, evidence-based programs and health professionals they need to live their healthiest, happiest and most productive lives. In addition to providing individual consumers with direct access to award-winning and innovative frictionless technologies, scientifically validated clinical protocols and best-in-class coaching tools, Sharecare also helps providers, employers and health plans effectively scale outcomes-based health and wellness solutions across their entire populations. To learn more, visit www.sharecare.com.
[i] The Sharecare Awards are operated through the Sharecare Foundation, a nonprofit entity that Sharecare established solely in support of this awards program.
What Science Says About Eating Dinner Together As A Family
As we head into the holiday season, with families celebrating and feasting together, here are some thoughts on how we might benefit from such family time, not just over the next days, but throughout the entire year.
For generations, eating dinner as a family has been a common daily occurrence in America, but as our schedules have become busier and technology has seeped into most aspects of our lives, fewer and fewer households sit down together at the table each night without distractions. In fact, a recent study found that 47 percent of those surveyed ate dinner together as a family less than they had when growing up – even though four out of five parents love eating together as a family and almost 80 percent want to make eating together a bigger priority.
We all have the vague idea that eating together is good for the family unit–but what can breaking bread together at the same table really do for you and your kids? Researchers have looked into it–and there’s really no downside to family dinner without screens.
Let’s take a closer look.
4 Ways Family Dinner Together Makes Life Better
Family dinner means kids eat better food.
A 2018 study published in Jama Network Open followed over 2,700 kids ages 14-24 living with their parents and reported on what they ate during dinner. Their findings revealed that teens and young adults who ate at the dinner table with their family consumed significantly more fruits and vegetables, significantly less fast food and take-outs, and significantly less sugar-sweetened beverages. Another study, which focused on younger kids, ages 9-14, found that children who ate dinner with their families got more nutrients, including fiber, calcium, folate, iron, and vitamins B, C, and E.
Family dinner means better family relationships.
It shouldn’t be surprising to hear that sitting together as a unit and sharing your day helps make people feel closer to each other. But just to be sure, 2006 study surveyed almost 100,000 12th graders across the country and found that families who ate dinner more frequently together reported better relationships with their mothers, fathers, and siblings. The teens also reported that they just liked having family dinner, with 71 percent claiming that talking and catching up with their family was the best part of eating together.
Family dinner means socially and emotionally healthier kids.
The study mentioned above also found that teens who eat more often with their family are less likely to engage in high-risk and destructive behaviors, including “substance use, sexual activity, depression/suicide, antisocial behaviors, violence, school problems, binge eating/purging, and excessive weight loss.” At the same time, kids with family dinner were more likely to express a “commitment to learning, positive values, social competencies, and positive identity.”
Family dinner means more academic success for kids.
Finally, family dinner is great for kids’ brain development and school performance. One study found that talking during family dinner helped kids’ literacy, from improving their vocabulary to developing storytelling skills and narrative comprehension. Finally, kids who eat with their family get better grades in school, according to the American College of Pediatrics.
How To Incorporate Family Dinner Into Your Life
Family dinners don’t have to be fancy or long–and you don’t have to have one every single night. The setting doesn’t matter, so go ahead and have it in your dining room or kitchen, or even at a restaurant. The food doesn’t have to be gourmet, either–though homemade is often healthier. Just make sure that there aren’t screens involved so that everyone is mentally present. If you don’t do family dinner at all, try starting with one night a week (one study found that Wednesday is the easiest place to start) and work up from there.
References
- Fulkerson, J. (2006). “Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors.” Journal of Adolescent Health. https://www.ncbi.nlm.nih.gov/pubmed/16919794
- Gillman, M. (2000). Family Dinner and Diet Quality Among Older Children and Adolescents. Arch Fam Med. http://triggered.edina.clockss.org/ServeContent
- Refrigerated and Frozen Foods. (2106). “Study Shows Trends in Family Mealtimes.” https://www.refrigeratedfrozenfood.com/articles/90952-study-shows-trends-in-family-mealtimes
- Snow, K. (2006). “Mealtime talk that supports literacy development.” New Directions for Child and Adolescent Development. https://onlinelibrary.wiley.com/doi/abs/10.1002/cd.155
- Walton, K. (2018). “Exploring the Role of Family Functioning in the Association Between Frequency of Family Dinners and Dietary Intake Among Adolescents and Young Adults.” JAMA Network Open. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2715616
What You Need To Know About E-Cigarettes, Vaping, and Your Teens
A Food and Drug Administration (FDA) survey released this month has found that e-cigarette use among high schoolers has increased by 78 percent just in the last year, while e-cigarette use among middle schoolers has increased by 50 percent.
The new data has health officials shocked–and taking immediate action against vaping companies that have practices that may appeal to teens and tweens. Following the release of the survey results, FDA Commissioner Dr. Scott Gottlieb resolved to crack down on e-cigarette companies that:
- Sell vaping flavors that appeal to kids, like mango, cream, and fruit medley
- Use advertising that appeals to the youth, such as young-looking actors or cartoons
- Sell e-cigarettes and pods online with lax restrictions
What is Vaping & E-Cigarette Use?
E-cigarettes are alternative nicotine delivery systems that allow smokers to inhale a vapor instead of smoke. Initially developed to help cigarette smokers move to a less harmful product on the road to quitting, it has been taken up by people who haven’t previously used tobacco products, most notably, teens. Not only that, but teens that start vaping are significantly more likely to start smoking down the road.
E-cigarette products consist of disposable e-cigarettes, rechargeable e-cigarettes, and refillable e-cigarettes. The most popular product among teens are small rechargeable, refillable JUUL brand vaping products which are small and easily concealable.
Understanding Teen Vaping
While traditional cigarette use is steadily falling among school kids, vaping is a novelty that many children simply don’t know the dangers of. Why is vaping suddenly increasing in popularity among teens? There are several factors at play:
- E-cigarettes can be easily concealed and used indoors.
- Children may not know that e-cigarettes contain nicotine or that they are addictive.
- E-cigarettes currently come in a variety of attractive flavors.
- Parents may not recognize what e-cigarettes look like–some, like JUUL, look like computer flash drives.
Could Your Adolescent Be At Risk To Start Smoking?
About 16 percent of teens try a nicotine product by the time they graduate high school–how can you know if your child might be at risk to start smoking? A five-year Canadian study of over 1,300 youth recently found that risk factors include:
- Kids who are friends with kids who smoke
- Kids who have tried drinking alcohol
- Kids who are friends with kids who drink alcohol
- Kids who are worried about their weight/appearance
- Kids who are worried about family relationships
- Kids who feel hopeless about the future
Resources For You And Your Teen
Thanks to the FDA crackdown, JUUL has agreed to greatly limit selling flavors and to shut down its social media presence. But while federal regulations on vaping products will help the epidemic, you can still play a role in making sure your own teen doesn’t start.
- A tip sheet for parents who want to talk to their teens about e-cigarettes, prepared by the Centers for Disease Control (CDC)
- Resources about quitting nicotine, from the U.S. Department of Health and Human Services
- More information about teen vaping
References
- Food and Drug Administration. (2018). Results from 2018 National Youth Tobacco Survey. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm625917.htm
- Leventhal, A. (2015.) Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA. https://www.ncbi.nlm.nih.gov/pubmed/26284721
- McMillen, R. (2018.) Adolescent Use of Different E-cigarette Products. Pediatrics. https://www.ncbi.nlm.nih.gov/pubmed/30201626
- Sylvestre, M. (2018.) A Tool to Identify Adolescents at Risk of Cigarette Smoking Initiation. Pediatrics. http://pediatrics.aappublications.org/content/142/5/e20173701.supplemental
Advice for Surviving the Holiday Season with Crohn's Disease
To mark Crohn’s and Colitis Awareness Week, we invited Kerianne Nosari to share her thoughts on living with Crohn’s disease throughout the upcoming holiday period.
My name is Kerianne and I was diagnosed with Crohn’s disease when I was 15 years old. You may have heard my story on the In My Words podcast which goes into detail on my journey through Crohn’s disease. If you haven’t heard it yet, make sure you check it out!
Living with Crohn’s disease can be embarrassing, scary and really hard to deal with at times. It can even get worse before it gets better. But it does get better! It’s important to remember that how you feel today isn’t how you are always going to feel. I had a moderate to severe case of Crohn’s disease before I had surgery, and now I am not on any medications, managing it through diet and lifestyle. Everyone’s experience is different. I think that’s a big factor to remember, but it’s also incredibly helpful to hear other people’s stories and how they deal with this condition.
Crohn’s disease is often triggered by diet and stress, two things that can be very present during the holidays. With the festive season approaching, I wanted to share how I manage my Crohn’s disease during periods like this. Christmas Eve is my favorite day of the year. It’s a day filled with joy, laughter and celebration with all the people I love. But it also comes with nervousness and apprehension when it comes to all the traveling and being around large crowds. The idea of being in the middle of a conversation with someone and feeling the rumbling in your belly knowing you need to excuse yourself right NOW, or traveling between destinations mapping out bathrooms along the way or even just trying to find something you can eat through all the goodies that are on the table, the day comes with a lot of stressful scenarios when living with Crohn’s disease.
When I first got diagnosed with Crohn’s disease the holidays were exhausting. My body would be completely worn down and it was really hard staying out places for more than an hour or two. Unfortunately when you first get diagnosed you don’t know what things affect your symptoms the most so you are playing the guessing game when it comes to food, which was one of my biggest anxieties. Now that I have been living with Crohn’s disease for over 10 years I have learned to try and avoid certain foods such as peanut butter, salad/raw vegetables, sweets, beef, spicy/greasy foods etc. I have also learned that it’s ok to indulge a little, because lord knows I love me some sweets! I just know now to really listen to my body and to not go overboard.
When it comes to the holidays, I have two rules.
Rule #1 – Eat before I go anywhere. This way I can control what is going into my body. Also, if I need to use the restroom, I don’t have the anxiety of someone knocking on the door as I am in the comfort of my own home.
Rule #2 – Bring something with me that I can eat. This is a great approach for two reasons: I am not coming empty handed and I have something I can eat wherever I go. I have been doing this for the past couple years and it has helped out tremendously.
If I can control even one part of a certain scenario when it comes to my symptoms, it’s a win for me. With the holidays quickly approaching, try testing out a couple things that you could possibly do to help yourself get through the holidays. You may even surprise yourself and find something that really works!
I hope that this is the best holiday season for you yet!
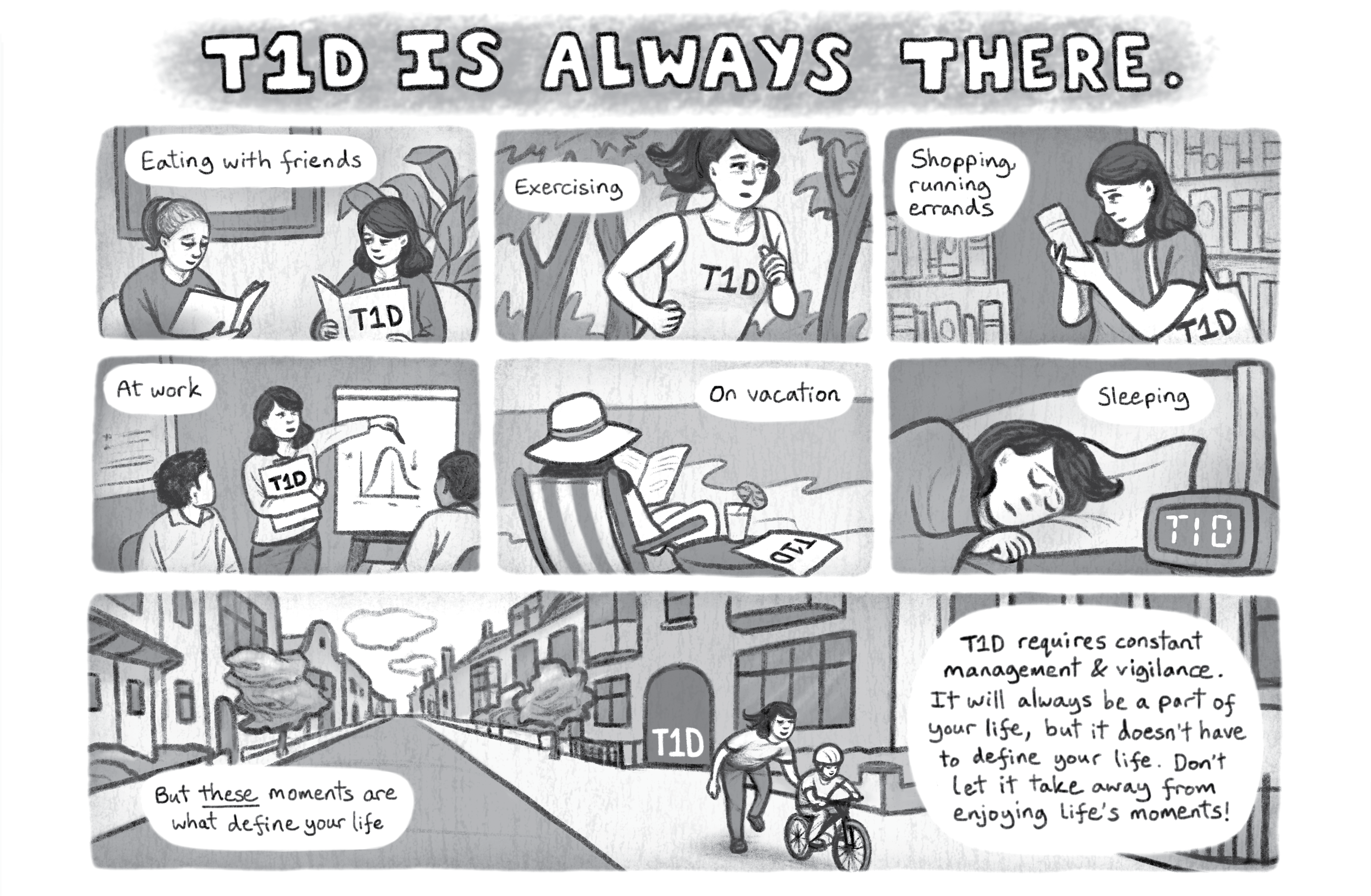
A Day In A Life With Type 1 Diabetes
To mark the end of Diabetes Awareness Month, we are delighted to share a mini-comic that highlights the experience of living with the condition.
Written by Erica Salerno-Sabastiani, PhD
Drawn by Katriona Chapman
Away With Epilepsy Founder Offers Advice for Teens
My name is Megan, and I have Juvenile Myoclonic Epilepsy. I was diagnosed with JME after I had two seizures in my parents’ bedroom New Year’s Day, 2013. I was 14 years old. When I was diagnosed, I had no one to talk to and no one to give me any wisdom they had learned from their own experience with epilepsy. I struggled a lot and had to learn “do’s” and “don’ts” on my own. My hope with this post is to share what I’ve learned with other teens who are struggling so they don’t have to go through the hardships I went through. Think of this as my “Teens With Epilepsy Cheat Sheet” if you will.
The first and foremost thing I want to share is that epilepsy can’t stop you from living your life. Yes, you will have seizures, maybe even quite often at first, but they will not stop you from living your life to the fullest it can be. If you sit there and wallow in self-pity for the rest of your life following your diagnosis, you’ll definitely miss out on the teen experiences life has to offer. As hard as it might be at first, you need to remember that you are still capable of doing things. You may have limitations, but with help from others and with motivation and drive coming from yourself, you can still do what you want to do and enjoy life.
Second thing: Take. Your. Meds. Don’t let the idea of “oh it’s just one dose. I’ll be fine” or “they don’t even do much anyway” lead you astray. Missing even one dose can be catastrophic. Your likelihood of having seizures increases and the likelihood of those seizures being deadly increases. Don’t risk it. Yes, side effects suck and relying on pills suck, but does it really suck more than being in a hospital or being dead? I don’t think so. I’ve been there and done that, and it was the worst decision of my life. If side effects are really bothering you, talk to your doctor. You’d be surprised to know how many medications are out there for treating epilepsy. I definitely was.
Last thing, don’t be afraid or embarrassed to ask for help or support. While I did do a lot of my learning alone, I also had help from my local support group. Hearing others’ experiences and being able to talk about things you can’t talk about with your parents or friends takes a big weight off of your chest and allows you to see that you’re not alone. Realizing that you aren’t alone in the fight really helps your mindset and can lift you up from the rock bottom you might be at. I know support groups in movies and TV look really stupid, but when done right they actually really help.
Additional Resources
- Epilepsy Resources from Jumo Health
- Read Megan’s Away With Epilepsy Blog
- Like Away With Epilepsy on Facebook
- Follow Away With Epilepsy on Instagram
Misconceptions About Obesity & Healthy Eating
Throughout recent history, we’ve gone through repeated cycles of dietary fads that shun certain types of food, including fats, carbs, and sugars. Corn Flakes, for example, were invented in 1894 as part of a low-fat diet craze, while the Atkins Diet, which shuns carbs and sugars, surged to popularity for the first time in 1974.
But are any of these dietary trends tied to real science about how what we eat affects obesity? A recent New York Times article explained that although diet has been studied extensively, there’s still not been a truly comprehensive, long-term study of the effects of diet on human obesity. We do have, however, a new study on mice that is shedding new light on the subject (and the results are surprising).
The Role of Fat In Obesity
A recent Cell Metabolism study followed lab mice on 29 different diets over a three-month period–which translates to a human being on a diet for nine years. The results even surprised the researchers: the only constant in the mice who became obese was a high-fat diet. In addition, mice on the high-fat diets also showed changes to their brains in the way that they processed rewards.
While this is only one study–and a study conducted on mice and not humans–it may show that consuming fat is closely linked to putting on fat, and while consuming sugars and carbs may have other negative health impacts, they may not be the main culprits when it comes to our waistlines.
Other Misconceptions About Obesity and Health
As research methods improve and our knowledge deepens, we are increasingly able to bust more and more myths about dieting and obesity. But even now, we have enough evidence to clear up some of the most common misconceptions. A 2013 special article in the New England Journal of Medicine outlined six such myths:
- Myth 1: Small changes in caloric intake or activity will result in large changes in body weight over time. In reality, making a small lifestyle changes can help you lose weight, but they won’t accumulate into large changes in weight as time goes by.
- Myth 2: It’s essential to set realistic weight-loss goals. Science actually shows that more ambitious goals are sometimes associated with better results, and that realistic goals don’t improve weight loss.
- Myth 3: Rapid weight-loss is associated with poor long-term results. Studies have shown that it isn’t necessarily bad to lose weight somewhat rapidly, when it comes to long-term outcomes.
- Myth 4: You have to be “ready” to lose weight. A study has found that if you would like to lose weight, you are ready enough to make changes.
- Myth 5: Physical education classes help prevent childhood obesity. While exercise surely affects the health of kids, in their current form, PE classes don’t significantly affect students’ BMI.
- Myth 6: Breastfeeding protects kids against obesity. While breastfeeding has other proven benefits, for mother and child, protecting kids against obesity has never been found to be one of them.
Two Constants: Activity and Moderation
Fad diets come and go–and even accepted science can change over time. But large bodies of research consistently point toward a combination of physical movement and moderation when it comes to health and healthy weight. Along with the busted myths above, it’s something to think about as the holidays approach.
References
- Casazza, Krista. (2013). “Myths, Presumptions, and Facts about Obesity.” New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMsa1208051
- Hu, Sumei. (2018) “Dietary Fat, but Not Protein or Carbohydrate, Regulates Energy Intake and Cases Adiposity in Mice.” Cell Metabolism. https://www.cell.com/cell-metabolism/fulltext/S1550-4131(18)30392-9
- Reynolds, Gretchen. (2018) “Which Kinds of Food Make Us Fat?” New York Times. https://www.nytimes.com/2018/09/25/well/eat/which-kinds-of-foods-make-us-fat.html?