Advancing Health Equity: Community-First Approach to Drive Diversity in Clinical Research
October 25, 2024 | In clinical research, one ongoing challenge continues to persist: a lack of diverse representation. While the root cause stems from a combination of limited access and endemic mistrust of the health care system among certain communities, the outcome is that large pockets of communities are often excluded from studies, even in key areas where they are disproportionately affected by diseases such as diabetes, heart disease, and certain forms of cancer.
However, new strategies are emerging to address this imbalance. Community-based approaches in clinical trials are paramount to bridging this gap and paving the way for more inclusive and effective healthcare solutions.
Understanding the Problem
The underrepresentation of diverse populations in clinical research is not just a matter of statistics. It means that certain communities may not fully benefit from medical advancements. For example, while African Americans represent about 13% of the U.S. population, they make up less than 8% of clinical trial participants. The consequences are clear: treatments may not be as effective for the populations not adequately represented in the research studies.
True health equity can only be realized in healthcare when relationships within the communities in question are established and nourished on an ongoing basis; just showing up once when an investigator need them to join a trial is a recipe for continued failure. Many communities, such as Black/African American, Hispanic/Latino, LBTQ++, American Indian/Alaska Native (AIAN), and Asian American and Pacific Islander (AAPI), face barriers to healthcare access and participation in clinical trials.
There are many reasons why underserved communities do not participate in clinical trials, but mistrust of pharmaceutical companies and healthcare providers, driven by historical injustices such as the treatment of Henrietta Lacks and the participants in the Tuskegee Syphilis Study, plays a significant role.
To address this issue, many research institutions are engaging local organizations and stakeholders to institute a community-based approach to improve awareness, education, trust, and ultimately participation in clinical studies.
The Role of Policy Makers
On June 26, 2024, the FDA provided guidance urging pharmaceutical companies and researchers to prioritize diversity with programs like the Diversity Action Plan (DAP). This approach helps to enrich the data collected, ensuring a more comprehensive understanding of how the treatment affects various patient populations. Increasing diversity in these studies helps gain deeper insights into the disease or therapy being examined to ensure that results are more broadly applicable.
Barriers to Diverse Participation in Clinical Studies
There are significant barriers that pharma companies must overcome when recruiting participants from underrepresented communities including cultural mistrust, potential language differences, and facilitating shared dialogue between healthcare providers and patients.
In addition, many minority populations face financial constraints, lack of reliable transportation and limited access to healthcare facilities. It can be difficult to attend appointments during work hours or find childcare during their appointment time. While solutions such as transportation services, patient payment solutions, and at-home nursing options can help mitigate these challenges, accessibility for these communities must be considered when the protocol is developed.
The Importance of a Community-Based Approach
To overcome these barriers, targeted solutions are needed to engage communities with healthcare education well before recruitment, address historical mistrust in medical research, and partner with culturally competent organizations. Tailoring interventions to community needs and working with trusted organizations can improve health literacy and reduce health disparities. It is also imperative to provide authentic, culturally relevant educational content, tools, and resources that speak to each unique community to bridge this gap.
When done right, these efforts can improve recruitment and increase retention rates, ensuring the representation of diverse populations.
Strategies for Implementing Community-Based Approaches
Effective strategies include:
- Partnering with credible local organizations who have roots in the community
- Utilizing community-based participatory research approaches
- Hosting informational sessions and micro-workshops in trusted community spaces like churches, community centers, hair salons
- Providing digital, video and print educational materials that are culturally relevant, easy to understand and actionable
Medical terminology is often overly complicated, and impossible to understand. A critical aspect of a successful community-based strategy is working with a specialized medical communication organization to create customized print, digital, and video content that is relevant, easy to understand, and practical.
Importance of Selecting Community-Based Trial Sites
Even when patients in an underrepresented community are properly educated on clinical trials and interested, it is often difficult for them to participate if there is not a trial site nearby. Establishing trial sites within the community and providing weekend or after-hours appointments can make participation significantly easier for these patients.
Diversity training for healthcare providers and site coordinators and inclusive educational resources can empower site staff to engage with patients from underserved communities. Employing principal investigators who reflect the community demographics is another way to help patients feel more comfortable in a clinical setting.
The Path Forward
If we are to create a healthcare system that truly serves everyone, clinical trials must reflect the diversity of the population. Community-based models are proving to be a powerful tool in achieving this goal, ensuring that medical advancements are informed by those who need them most. By investing in local engagement, addressing common barriers, and building trust, the medical community can take meaningful steps toward a future where access to clinical trials truly is equitable. The hope is that more communities will benefit from medical research, improving health outcomes, and narrowing the gaps in healthcare access and quality.
Creating Inclusive Clinical Trials
The push to increase diversity in clinical trials has gained momentum, but true progress requires more than regulatory mandates. It involves building trust, fostering authentic relationships and amplifying the voices of those most impacted by health inequities.
While the pharmaceutical industry has made strides in improving patient diversity in clinical trials, our recent webinar moderated by Kevin Aniskovich, CEO of Jumo Health, underscored that much work remains to ensure trials are truly inclusive and representative of all populations.
In this webinar, we were joined by industry leaders and patient advocates who discussed how authenticity and the patient voice can be leveraged to enhance diversity in clinical trials. The panel shared powerful insights on the role of storytelling, community engagement and long-term partnerships in driving meaningful change.
The discussion outlined actionable strategies that pharmaceutical companies, community leaders and patient advocates can use to build trust and inspire participation from underrepresented communities.
“What better legacy could I leave for my children, my grandchildren and future generations than to get involved, to actually create a better world that I want, and we all want, and deserve to live in, and you can only do that by being involved.”
— Tony Wafford
Authenticity as the Foundation of Trust in Clinical Research
Diversity in clinical trials cannot be achieved overnight. As webinar panelist Tony Wafford, President & CEO of I Choose Life Foundation, emphasized, “It is a journey, not a moment.”
At the heart of this journey is authenticity, which requires the pharmaceutical industry to meaningfully engage with underrepresented communities, understand their unique challenges and build trust through transparent, culturally sensitive communication.
This goes beyond delivering a well-crafted message—it involves truly listening to communities, addressing their concerns and overcoming the specific barriers they face in participating in clinical trials.
Wafford highlighted that authenticity leads to trust, and trust leads to action. For the pharmaceutical industry, this means being present in the communities long before recruitment starts, establishing relationships based on mutual respect and showing a sincere commitment to health equity.
“It’s not enough to just say, ‘Here’s a clinical trial, you should consider it.’ We need to educate and empower people, ensuring they feel safe and supported throughout their journey.”
— Michele Falk
Community Engagement: A Critical Component
Building trust and improving trial diversity requires meeting communities where they are—both literally and figuratively. Engaging trusted community leaders and organizations with an established presence in the area can be an effective way to introduce conversations around clinical trials in an environment where people feel safe and understood.
“We learn from both our victories and the challenges and barriers we encounter along the way,” said Michele Falk, Senior Manager, Patient Engagement & Recruitment Lead at Bristol Myers Squibb.
She emphasized that building trust isn’t a one-time effort but requires a sustained presence, listening to community needs and adapting strategies based on feedback.
Falk also pointed out that diversity initiatives cannot be top-down efforts, where the pharmaceutical industry simply introduces clinical trials into a community. Instead, these initiatives must involve the community from the ground up.
For example, community action boards, made up of individuals who are representative of their communities and committed to advocating for health equity, can help guide strategies that are culturally appropriate and tailored to the specific needs of the population. This collaborative approach addresses historical mistrust while ensuring that diversity efforts are meaningful and part of a larger, sustainable movement, rather than merely token gestures.
“I needed other people who look like me—especially African American women, who have the highest mortality rates from breast cancer, specifically triple-negative breast cancer—to know, ‘This is what happened to me.'”
— LaToya Bolds-Johnson
The Power of Patient Voices in Changing the Narrative
One of the most effective ways to increase participation in clinical trials is by elevating the voices of those who have experienced them firsthand. Patient stories create emotional connections. Stories can also help dismantle the perception that clinical trials are intimidating.
When individuals hear from others who share similar experiences—especially those from their own communities—the process can become more relatable and less overwhelming.
LaToya Bolds-Johnson, a breast cancer survivor and passionate patient advocate, shared her personal journey navigating clinical trials. Her story highlights how even those with medical expertise can face barriers to accessing trials. “I realized very early in my chemotherapy journey when I was asking to be part of clinical trials, that I was being dismissed,” she recalled.
Despite her medical background, LaToya encountered significant challenges in finding and enrolling in a trial. She noted, “I was literally sending my oncologist clinical trials that I found. Most people don’t know how to do that. If you go on the clinical trials website, it’s very complicated. Even healthcare providers struggle with the terminology and complexities.”
Diagnosed in 2021 with stage 3C triple-negative breast cancer, LaToya’s experience inspired her to become an advocate through her nonprofit, The Tatas 365, which raises awareness about early breast cancer screening for high-risk Black women.
LaToya’s persistence in advocating for herself underscores the broader issue of access and inclusion in clinical research. Her story illustrates the challenges many patients face, particularly those from underrepresented communities, and highlights the critical need for the healthcare industry to actively listen, engage and support diverse patient populations.
“The importance of storytelling and the power of the patient’s voice can serve as a means to not only drive health literacy, but more engagement and participation in clinical trials.”
— Kevin Aniskovich
How Patient Stories Can Create a Lasting Impact
Storytelling is one of the most effective ways to connect with potential clinical trial participants. It’s an age-old method of communication that fosters understanding and empathy. For clinical trials, storytelling can cut through the uncertainty and fear surrounding the process.
When patients like Bolds-Johnson share their authentic experiences, it resonates with others who may be facing similar health challenges and concerns about trial participation.
Gwen Oakes, Director of Global Trial Optimization at Merck, emphasized the power of stories in making clinical trials more relatable and accessible to a broader audience. By featuring real stories from diverse patients through video and educational content on their clinical trials website, Merck aims to make the clinical research process accessible to all people.
“We want to make sure that people have access, that they have awareness and that they have education.”
— Gwen Oakes
Overcoming Barriers to Participation
Access to clinical trials remains one of the biggest barriers to participation for underrepresented communities. These challenges range from logistical issues, such as travel distance to trial sites, to a lack of awareness being provided about the clinical trial process. Even when patients are informed, navigating the complex enrollment systems can be overwhelming.
Bolds-Johnson’s experience of having to fight for her inclusion in a trial—even with a medical background—highlights the difficulties that many patients face. For those without a healthcare background, navigating clinical trial information can be even more daunting.
Falk emphasized the need for education and bridging gaps, not just for patients but for healthcare providers as well.
“We need to build those pathways. Those streets don’t exist,” she said, pointing out that both healthcare providers and patients often lack the information they need to connect with clinical trials. Educating providers on available trials within their own geographic regions can help ensure that patients are referred to appropriate studies, increasing overall participation and diversity in trials.
In addition to education, community engagement plays a crucial role in overcoming participation barriers. As discussed in the webinar, community action boards can foster trust and improve trial diversity. These boards, made up of individuals from the communities being approached for clinical trials, can guide strategies to ensure they are culturally appropriate and responsive to the specific needs of the population.
By involving local leaders and advocates, the industry can create stronger connections with communities and develop initiatives that resonate on a personal level.
For pharmaceutical companies, this also means developing clearer, more accessible resources that make it easier for both patients and healthcare providers to understand the clinical trial process. Simplifying medical jargon and offering educational materials in multiple languages are small but important steps toward increasing inclusion.
By leveraging community action boards and improving trial information accessibility, the industry can help individuals make informed decisions about participation.
“Not one of us has all the answers, but the answers rest within us all.”
— Kevin Aniskovich
Collaboration and Partnership for Real Change
Making clinical trials more diverse, equitable and inclusive isn’t something that can be done in isolation. It requires collaboration across the pharmaceutical industry, regulatory bodies, patient advocates, healthcare providers, community leaders and more.
As the webinar panelists pointed out, no single group has all the answers, but together, we can all make meaningful strides toward more inclusive clinical trials. There is no one-size-fits-all solution to this issue. Each community is unique, and the strategies for engaging with them must be tailored accordingly.
Authentically elevating diverse patient voices and pursuing community engagement are critical to this process. By building trust, fostering long-term relationships and making the clinical trial process more accessible, the pharmaceutical industry can ensure that research reflects the diversity of the populations it aims to serve.
In Their Shoes: Breast Cancer Edition
Personal stories matter.
They mean a lot to patients, caregivers, and loved ones, as they can bring comfort to those feeling alone in their breast cancer journey. We’re excited to kick off a new blog series called In Their Shoes: Breast Cancer Edition! Each week, we’ll share real stories from amazing people living with breast cancer.
We hope these experiences help you feel connected and supported. Stay tuned for heartfelt stories that will remind us that no matter what we’re going through, we’re not alone!

I’m Denise McCrossin, and this is my story.
I had everything ahead of me in the mid-90s. I was a mom of four who loved traveling, playing tennis and racketball, and hiking. Then, in 1998, I was hit with the news that I had breast cancer.
At the time, I was terrified I would die. Then, after what I call my initial “pity party” at hearing I had cancer, I shifted my attitude and went into treatment with a more hopeful attitude. Part of my treatment at the time involved numerous scans, a lumpectomy, the removal of nodes, and, eventually, a mastectomy.
Although treatment wasn’t easy, I tried to keep my life and the lives of my family as normal as possible. I even volunteered for an organization called “Reach To Recovery,” where I would visit and talk to others about what I had been through to help them not feel alone on their journey.
As with most cancers, there is a chance that the cancer can come back. Sadly, that has been the case for me. This time around, nearly twenty-six years later, I will start treatment again, except I will be undergoing bio-therapy as well as chemotherapy and surgery.
My advice to others recently diagnosed with breast cancer is to know that breast cancer isn’t a death sentence anymore. So, stay active and keep your life as normal as possible. For those who are caregivers of someone with breast cancer, offer to take them to their treatment appointments, cook meals, buy gift cards to their favorite restaurants, and help them leave the house by taking them places they enjoy.
The most important advice I can give, whether you have breast cancer or you’re someone’s caregiver, is to stay positive, remember you’re not alone in this, and not be afraid to ask for help if you need it.
We hope these experiences help you feel connected and supported. Stay tuned for heartfelt stories that will remind us that no matter what we’re going through, we’re not alone!

I am Jennifer Johnson, and this is my story.
I was 38 years old and in the best shape of my life. As an avid hiker, runner, and fitness instructor, I had built a lifestyle around health and wellness, so when I was diagnosed with triple-negative breast cancer, I was stunned. With no family history of breast cancer, I never expected that this disease could affect me. I felt invincible, constantly pushing my body to new limits, whether running marathons, leading fitness classes, or hiking new trails.
The day of my diagnosis, everything changed. I had gone in to see my doctor after finding a lump in my breast; I knew something wasn’t right. I advocated for a mammogram despite the recommended guidelines of waiting until 40 years old.
After getting scanned and then having the lump biopsied, I remember sitting in my doctor’s office completely blindsided. How could someone so focused on health and fitness have cancer? It didn’t make sense. That moment of disbelief quickly transformed into determination. I decided that, just like any other challenge I had faced, I would take this one head-on.
My daily routine shifted from teaching fitness classes to balancing chemotherapy
sessions, tracking medications, and still finding time to stay active in ways that my body would allow. Movement had always been a source of strength for me, and even on the
most challenging days, a walk in nature or a gentle yoga session would help me feel a bit more like myself.
What got me through this time was my commitment to staying active and the overwhelming support from my community. My friends, family, and fellow hikers rallied behind me. They reminded me that I wasn’t fighting alone. That encouragement and my passion for fitness became my anchors during the toughest parts of treatment.
If I could offer one piece of advice to others facing a similar diagnosis, it’s to find what makes you feel strong and hold onto it. Whether it’s fitness, art, or time with loved ones, having something to focus on outside of your diagnosis can make all the difference. Today, as a survivor, I continue to advocate for health and fitness, knowing that every step forward is a victory.
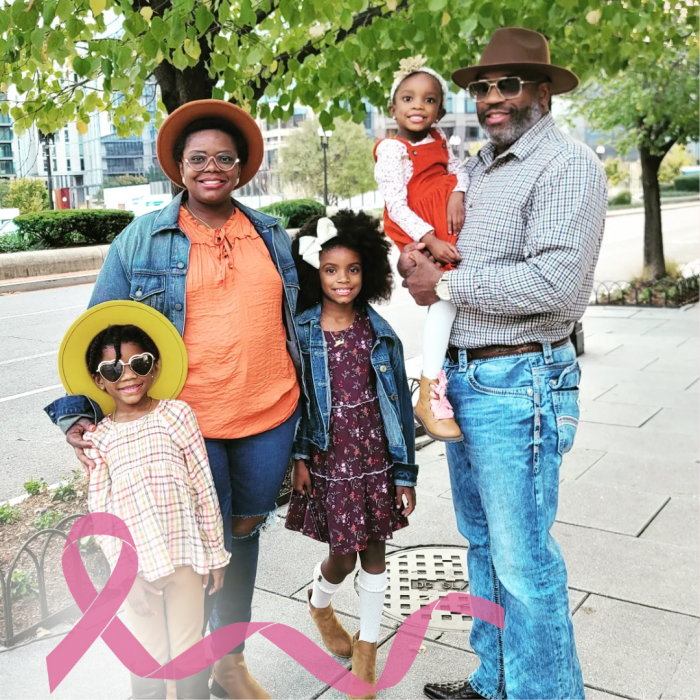
I am LaToya Bolds-Johnson, and this is my story.
I had felt a lump in my left breast about a month before my diagnosis. I didn’t think there was any significance after discovering the lump. I had not long ago stopped breastfeeding my one-year-old baby girl at the time, and I just figured it was a residual breastfeeding milk cyst. A couple more weeks passed by, and I still felt a lump, so I set up a virtual appointment and was able to have a mammogram and sonogram scheduled.
Then, on July 26, 2021, while I was working in the emergency department on a 12-hour shift, I received the devastating news of a cancer diagnosis on my phone through a patient portal email alert. I looked at the report and read the pathology findings showing triple-negative breast cancer, grade 3.
It took me a long time to process that I was actually a cancer patient. How could this be? I am a licensed healthcare professional. I am the person who takes care of patients; how did the roles flip? That was the biggest part of it all for me to digest, and I felt vulnerable and weak.
After about 8 weeks of chemo, an epiphany came to me. I felt helpless but wanted to do something to still help patients during my cancer treatment journey. The healthcare provider was still alive within me, and I needed to do something to make me feel fulfilled in some way. I decided to start posting videos about my diagnosis in hopes that it would reach another woman who looks like me and is the same age.
I felt people needed to know they should not wait until their 40th birthday for a mammogram. Get a mammogram now! Early detection saves lives. No one pushed this health recommendation to me, and even through my PA college education, I was always taught mammograms don’t start until age 40. Well, the recommendations and those schoolbooks were wrong.
My advice to others navigating breast cancer: Don’t forget to fight and count your blessings because you are blessed, my lovelies. Lose yourself in helping others feel better, and always be kind to yourselves. Remember, cancer is not just a physical diagnosis. It also affects your mental, emotional, spiritual, and financial state. It also affects your loved ones, and as a cancer thriver, you definitely need a support system and mental health treatment, too. I have good and bad days, but I’ve dedicated myself to helping to eradicate breast cancer and decrease the higher mortality associated with Black Breast Cancer. I owe this new mission in my life to my three daughters, whom I pray will never have to experience what I am going through in this journey of life.
The day of my diagnosis, everything changed. I had gone in to see my doctor after finding a lump in my breast; I knew something wasn’t right. I advocated for a mammogram despite the recommended guidelines of waiting until 40 years old.
After getting scanned and then having the lump biopsied, I remember sitting in my doctor’s office completely blindsided. How could someone so focused on health and fitness have cancer? It didn’t make sense. That moment of disbelief quickly transformed into determination. I decided that, just like any other challenge I had faced, I would take this one head-on.
My daily routine shifted from teaching fitness classes to balancing chemotherapy
sessions, tracking medications, and still finding time to stay active in ways that my body would allow. Movement had always been a source of strength for me, and even on the
most challenging days, a walk in nature or a gentle yoga session would help me feel a bit more like myself.
What got me through this time was my commitment to staying active and the overwhelming support from my community. My friends, family, and fellow hikers rallied behind me. They reminded me that I wasn’t fighting alone. That encouragement and my passion for fitness became my anchors during the toughest parts of treatment.
If I could offer one piece of advice to others facing a similar diagnosis, it’s to find what makes you feel strong and hold onto it. Whether it’s fitness, art, or time with loved ones, having something to focus on outside of your diagnosis can make all the difference. Today, as a survivor, I continue to advocate for health and fitness, knowing that every step forward is a victory.
I am Michelle Gordon, and this is my story.
In the early 90s, I loved dancing and music and all the things 11-year-olds do. I was a typical kid except for one thing: my mother had breast cancer. My mother was the first in the family that we know of to be diagnosed with breast cancer. One of my memories of that time is telling my parents that I wanted them to be honest with me about the results and any news.
I remember how scared I was when the doctors officially diagnosed her with breast cancer, but I also remember how grateful I was that my parents were honest with me about what was going on with my mother’s health. They gave me updates and explained the results, even when it wasn’t good news.
They also made sure that I saw a therapist. Seeing a therapist helped me talk about my worries without feeling like I was burdening my parents while they were dealing with my mom’s diagnosis, surgery, and treatment too.
Due to my mother’s diagnosis of breast cancer, my doctor recommended that I get screened earlier. So, while most women don’t get screened until they turn 40, I started getting screened a lot earlier than that—about 10 to 15 years earlier. A few of my scans have required biopsies to investigate unusual masses, but I’m so grateful that I’m consistent with getting screened, as screening and early detection can save lives.
The best advice I can give is to find a way to be as open as possible with your child in an age-appropriate way so that they won’t feel so in the dark about what’s going on. And if you’re able, see if your child would benefit from talking to a therapist. It really can help them process it all.
Then, on July 26, 2021, while I was working in the emergency department on a 12-hour shift, I received the devastating news of a cancer diagnosis on my phone through a patient portal email alert. I looked at the report and read the pathology findings showing triple-negative breast cancer, grade 3.
It took me a long time to process that I was actually a cancer patient. How could this be? I am a licensed healthcare professional. I am the person who takes care of patients; how did the roles flip? That was the biggest part of it all for me to digest, and I felt vulnerable and weak.
After about 8 weeks of chemo, an epiphany came to me. I felt helpless but wanted to do something to still help patients during my cancer treatment journey. The healthcare provider was still alive within me, and I needed to do something to make me feel fulfilled in some way. I decided to start posting videos about my diagnosis in hopes that it would reach another woman who looks like me and is the same age.
I felt people needed to know they should not wait until their 40th birthday for a mammogram. Get a mammogram now! Early detection saves lives. No one pushed this health recommendation to me, and even through my PA college education, I was always taught mammograms don’t start until age 40. Well, the recommendations and those schoolbooks were wrong.
My advice to others navigating breast cancer: Don’t forget to fight and count your blessings because you are blessed, my lovelies. Lose yourself in helping others feel better, and always be kind to yourselves. Remember, cancer is not just a physical diagnosis. It also affects your mental, emotional, spiritual, and financial state. It also affects your loved ones, and as a cancer thriver, you definitely need a support system and mental health treatment, too. I have good and bad days, but I’ve dedicated myself to helping to eradicate breast cancer and decrease the higher mortality associated with Black Breast Cancer. I owe this new mission in my life to my three daughters, whom I pray will never have to experience what I am going through in this journey of life.
The day of my diagnosis, everything changed. I had gone in to see my doctor after finding a lump in my breast; I knew something wasn’t right. I advocated for a mammogram despite the recommended guidelines of waiting until 40 years old.
After getting scanned and then having the lump biopsied, I remember sitting in my doctor’s office completely blindsided. How could someone so focused on health and fitness have cancer? It didn’t make sense. That moment of disbelief quickly transformed into determination. I decided that, just like any other challenge I had faced, I would take this one head-on.
My daily routine shifted from teaching fitness classes to balancing chemotherapy
sessions, tracking medications, and still finding time to stay active in ways that my body would allow. Movement had always been a source of strength for me, and even on the
most challenging days, a walk in nature or a gentle yoga session would help me feel a bit more like myself.
What got me through this time was my commitment to staying active and the overwhelming support from my community. My friends, family, and fellow hikers rallied behind me. They reminded me that I wasn’t fighting alone. That encouragement and my passion for fitness became my anchors during the toughest parts of treatment.
If I could offer one piece of advice to others facing a similar diagnosis, it’s to find what makes you feel strong and hold onto it. Whether it’s fitness, art, or time with loved ones, having something to focus on outside of your diagnosis can make all the difference. Today, as a survivor, I continue to advocate for health and fitness, knowing that every step forward is a victory.
The Power of Patient Stories: Blood Cancer Awareness Month
Believe it or not, there are more than 100 different types of blood cancer, with each one falling into one of three main types of blood and bone marrow cancers: leukemia, lymphoma, and myeloma. Treatments vary depending on what type of blood cancer a person has and at what stage their cancer was discovered.
Here’s a breakdown of the different types of blood cancer:
Leukemia
Leukemia is caused by the body’s rapid production of abnormal white blood cells in the bone marrow. When the body makes too many abnormal white blood cells, it hinders the bone marrow’s ability to make healthy blood cells. Leukemia is also the most common type of blood cancer in the United States and the most prevalent in children and teens.
Lymphoma
Lymphoma affects the lymphatic system, which is part of the immune system that helps defend the body against sickness. The two main types of lymphomas are non-Hodgkin lymphoma and Hodgkin lymphoma. Hodgkin lymphoma is far less common than non-Hodgkin and is characterized by a specific type of cell called a Reed-Sternberg cell.
Myeloma
Myeloma (multiple myeloma) is a blood cancer that starts from abnormal plasma cells in the bone marrow. Plasma cells are a type of white blood cell that usually fights infection. With myeloma, there are many abnormal plasma cells, called myeloma cells, which means the body can’t work as it should.
Blood cancers, which are mainly caused by DNA mutations, account for 10% of all diagnosed cancers in the US each year, and childhood leukemia accounts for about 25% of all cancers in children. In the UK, over 650 children and young adults are diagnosed with leukemia every year. (YaleMedicine.org, BloodCancer.org/UK)
Navigating Blood Cancer Diagnosis & Treatment
For parents, finding out a child has blood cancer can be both devastating and scary. Navigating your child’s journey with blood cancer can be incredibly challenging, but there are some ways to make this time a little easier. First and foremost, building a strong and open relationship with your child’s healthcare team is key. By sharing how your child is feeling and what’s happening, you’ll ensure that everyone is working together to provide the best care possible.
It’s also important to acknowledge your child’s feelings and celebrate their accomplishments, no matter how small. Your support and praise can make a big difference in their emotional well-being and help them feel more confident and hopeful.
Another valuable way to support your child is by connecting with others who understand what you’re going through. Joining a support group can provide both you and your child with a sense of community and understanding.
Connection Through Relatable Patient Stories
Listening to stories from other children who have faced similar challenges can be a powerful source of comfort and reassurance, helping patients and their families feel less alone on this journey. They provide a sense of connection and relatability that children undergoing cancer treatment often miss. Hearing these stories can also be extremely beneficial for siblings and other children in the family as these stories can help them process what’s happening in an accessible way. They can also help make sense of complex emotions and situations, fostering empathy and understanding.
One of the things we’re most passionate about is telling patient stories. In one of our custom “In My Shoes” videos, we met with Alistair, a young adult diagnosed with leukemia in his late teens. “On the day I found out I had leukemia, I guess it was a bit of a shock,” he recalled. It was the first time he needed to be hospitalized, and the experience was scary. Luckily, he had an incredible care team that helped him understand what was happening inside his body and what their plan would be for his treatment. “My advice for someone being newly diagnosed [would be to] ask your doctor any question you have about the treatment. [It] gave me a bit of comfort knowing what their plan was, knowing it was okay to ask for help. It’s okay to be scared and sad at times.” He went on to say that one of the biggest lessons he took away from this experience was that he could mentally push through it and stay positive.
If you’d like to learn more about how we create our custom “In My Shoes” videos, visit jumohealth.com or contact us.
Albertus Magnus College Receives Generous Donation From Jumo Health
New Haven, CT, September 16, 2024 – Albertus Magnus College is pleased to announce it has received a generous donation of Apple iPads® to its Nursing Program from Jumo Health, a global medical communications firm, headquartered in New Haven, Connecticut. This contribution aims to support and elevate the educational experience of nursing students at the College, ensuring they have access to essential digital resources as they pursue their degree.
Albertus Magnus College’s Nursing Program, known for its commitment to producing highly skilled and compassionate healthcare professionals, will use the iPads inside and outside the classroom — including in the new state-of-the-art nursing labs — as well as in the library and the Germain Learning Center. These devices will enhance students’ learning opportunities, providing them with tools for accessing medical databases, educational apps, and online research materials that are crucial for their training.
“We are incredibly grateful for Jumo Health’s donation. The iPads will significantly enrich our students’ learning experience and provide them with the technological education they need to succeed in today’s rapidly evolving healthcare environment,” said Cynthia Jeffrey, Ed.D., M.S.N., R.N., the College’s Nursing Programs Director. “Jumo Health’s support underscores the vital role that community partnerships play in advancing education and improving health literacy.”
Jumo Health’s donation reflects its ongoing commitment to improving education through technology, focusing on empowering communities and fostering future generations of healthcare professionals. The company continues to seek ways to contribute positively to the community and promote health literacy on a wider scale, reflecting the core tenets of its business.
“Jumo Health is committed to promoting health care in all its forms,” shared Kevin Aniskovich, President and CEO of Jumo Health. “Supporting Albertus Magnus College’s Nursing Program not only underscores our commitment to collaborating with our community institutions, but ensures future health care professionals train on, and become familiar with, the tools they will ultimately use in the field,” concluded Aniskovich.
About Albertus Magnus College
Albertus Magnus College, founded in 1925, is a coeducational Catholic College in the Dominican tradition. As New England’s most diverse Catholic College, Albertus’ values- and liberal arts-based education is recognized by external rankings such as US News & World Report, Money Magazine, and The New York Times, and has been named a Top 10 Military Friendly School. For eight consecutive years, at least 95% of Albertus graduates have attained full-time employment or gone onto graduate studies within six months of completing their degrees. The College has an enrollment of approximately 1,300 students across its traditional undergraduate, accelerated adult undergraduate, and 12 graduate programs. Proud to enroll a student body where more than half of its students come from minority backgrounds with nearly the same percentage of undergraduates receiving Federal Pell Grants and being first generation college goers, Albertus is known for its innovative curricular offerings, recently launching new Bachelor’s degree programs in Nursing General Health Sciences, Interdisciplinary Studies, Public Health, and Supply Chain Management; among its graduate programs is the State of Connecticut’s only Master of Arts in Art Therapy and Counseling program and just one of three schools to offer a Master of Science in Human Services. Just a year from its historic 100 th Anniversary, the College is implementing its Albertus 2025: Lighting the Way to a Second Century strategic plan, which articulates an inspiring, bold vision to “be a destination liberal arts-based college, distinguished in its interdisciplinary and experiential approach to education, rooted in Dominican values, that prepares students for lifelong civic engagement and success.” To learn more, please visit albertus.edu
Educational Materials That Make a Difference
How One of Our Comic Books Helped a Teen Discover She Had VKC
In July, the Jumo Health team had the honor of attending the International Children’s Advisory Network’s (ICAN) Annual Summit as the Champion Sponsor. During the event, we had the opportunity to speak with a teenager named Muminah, who is living with vernal keratoconjunctivitis (VKC).
Muminah shared an incredible piece of feedback with us. After many doctor visits and several misdiagnoses, it was finally a comic we created about VKC that ultimately helped her accurately identify what was wrong with her eyes.
According to the National Institutes of Health (NIH), vernal keratoconjunctivitis is a rare condition characterized by inflammation of the conjunctiva, the eye’s outer membrane. This inflammation can cause redness and blurred vision and, over time, may lead to a grayish discoloration of the retina. Muminah mentioned experiencing all of these symptoms. “I went home one day from school because all of my friends were asking me, “What’s wrong? Why are your eyes so red?” Their comments made her feel as though her friends only saw her eyes when they looked at her. This feeling negatively affected her self-esteem.
“I was nine years old, and I remember searching VKC and a health video came up of a comic and a boy who wanted to go outside. After watching that, it kind of made me feel like I wasn’t alone. I was like, that’s me!”
As a company, it’s incredibly fulfilling to hear how our work has a tangible impact on individuals. When Muminah shared how the comic helped her understand her condition better and feel validated in an emotional and psychological way, she underscored the importance of what we do and why.
Hearing stories like Muminah’s reinforces the dedication and care we put into every project. These moments remind us why we are so passionate about our work and its potential to make a real difference.
To hear Muminah’s story in her own words, view the video below:
3 - 2 - 1 ACTION: The Art of Live-Action Videos for Sharing Patient Stories
When patients and their support systems share their experiences, it humanizes health conditions, making them more relatable and impactful. Personal stories also help foster a deeper emotional connection between the audience and the subject matter.
Jumo Health’s signature “In My Shoes” videos provide invaluable insights into the real-life implications of a condition or treatment, illustrating the challenges and triumphs that aren’t always evident in data alone. By highlighting individuals’ journeys, we can create a more empathetic and comprehensive understanding of the condition, ultimately driving greater engagement, support, and advocacy.
Furthermore, personal stories can offer hope and encouragement to others going through similar experiences, demonstrating that they aren’t alone and have a path forward. This emotional resonance can be incredibly powerful for those considering joining a clinical trial and the broader community.
To get a glimpse into our process, keep reading!
The Process Behind Creating An Impactful “In My Shoes” Patient-Story Video:
Prepping For The Shoot
We start the process for every “In My Shoes” video by talking through the video so that everyone involved clearly understands the overall purpose. Once we fully grasp the need, medical writers begin crafting interview questions. Questions include a person’s hobbies and interests, their experiences before and after diagnosis, and if they have any advice to share. By asking these types of questions, we better understand the person we’re featuring beyond their medical condition.
One of our senior medical writers, Erica Salerno-Sabastiani, said, “I love working on projects like this. As a person with chronic medical conditions and the caregiver of a child with chronic medical conditions, I believe it’s important to get personal stories out there to raise awareness, stir empathy, and remind people that everyone’s struggling with something, even if you can’t see it.” She added, “Our videos also help validate caregivers’ experiences, and that’s just as important.”
Shoot Day
Our team is usually the first to arrive at the location on the day of the shoot. We use this time to ensure the equipment is set up correctly. By the time we’ve adjusted the lights, completed a soundcheck, and framed our picture, the participants have arrived, and we’re ready to break the ice and get started. Jesse Jankewicz, Director of Videography & Animation, goes out of his way to set everyone at ease, “I usually meet with the participants as soon as they arrive and just chit chat for a bit to get them comfortable with me. I’ll try to make some jokes or lighthearted quips about what we’re doing just to keep the mood light.”
This lighthearted banter relaxes the overall vibe of the set. It also opens up the participants in a natural way so that when they’re answering the questions, it feels more like a conversation versus a straight interview. “The most fulfilling part of my job is being able to tell someone’s story. I love meeting and talking with people. Many of the people we serve have had to overcome tremendous obstacles in their lives. It’s a privilege to be able to share their stories through a visual medium.”
When the interview portion of the video is complete, Jesse and his team tackle capturing b-roll. B-roll is footage that typically depicts elements of the story a participant shares, or shows the participant in their daily life. “We try to capture b-roll that’s unique to the person or re-enact a part of the story they’re telling,” Jesse said.
Editing It Together
When the footage is captured, we get the complete transcription of everything said during the day of filming. The transcription itself can be up to 50 pages. To trim the content down to the allotted time of the video, typically between two and five minutes, our Director of Creative Copy, Rachel Wilson, and our editor, Riley Brunner, go through every line, pulling out the key scenes that bring the participant’s story to life.
Rachel begins by reviewing each piece of captured dialogue before trimming it down word-for-word until it tells a cohesive, heartfelt story. “When going through the transcripts I look for those pivotal storytelling moments that speak to the heart of a person’s experience.”
Meanwhile, our editor, Riley, looks at the raw footage from a visual storytelling perspective, looking at the interview portion of the footage as well as any b-roll captured. B-roll is the unsung hero of most videos. It also gives the viewer a visual break and helps to keep them engaged. “Sometimes it’s hard to edit a story together that we don’t have any actual footage of, so we rely on B-roll to fill in some of those gaps with imagery that matches the person’s emotion as they’re telling us their story.”
Finishing the Video
Once the raw footage is cut together, Riley begins her music search. The right music drives the story forward and keeps the video engaging. “Like any good plot, music usually has a beginning, middle, and end–even if it’s just three minutes. If you can select music that builds with the story, then you’re adding a level of depth that really keeps people engaged. From an audience perspective, music helps set the tone for a video.” The result is a video that resonates with patients, their caregivers, and the community, helping to bring awareness about a specific condition or disease to more people.
What Participants & Clients Are Saying
A very special participant in one of our “In My Shoes” videos, LaToya Bolds-Johnson, featured in a video for a clinical study researching breast cancer, has been an ally and advocate for diversity in clinical trials and telling patient stories. For her, being in a clinical trial is like “a medical trust fund for my three daughters. If my body is researched, then I know my DNA is studied in an effort to help reach a goal to end TNBC (triple negative breast cancer) for my daughters and future generations.”
Amy Vassel, Clinical Program Leader, U.S Medical Affairs, Oncology Clinical Operations at Genentech, shared her thoughts on the “In My Shoes” video LaToya was a part of, “Shooting the video with Jumo Health was special because of the professionalism, creativity, patience, and the care that the Jumo Health team took that day. This video highlights the importance of listening to patient stories. LaToya’s incredible story taught us what we as an industry need to work on to ensure patients like her are offered the opportunity to participate in clinical trials.”
Receiving feedback like this is incredibly important to our team. We believe that genuine patient stories have the power to raise awareness about conditions and offer solace to others going through similar experiences, and our multidisciplinary team has the skills, compassion and vision to bring these stories to life.
To learn more about our video capabilities, check our website or message us by clicking here.
Falfurrias Management Partners Announces Investment in Jumo Health, An Innovative Clinical Trial Solutions Platform Driving Better Health Outcomes
CHARLOTTE, N.C., August 19, 2024 – Falfurrias Management Partners (Falfurrias), a Charlotte-based private equity firm focused on growth-oriented, middle-market businesses, today announced its investment in Jumo Health, an innovative and award-winning clinical trial solutions company driving better outcomes for clinical trials globally. Jumo Health develops creative, patient-centric educational solutions that improve health literacy to accelerate clinical trial enrollment and increase participant retention.
While clinical trials suffer from low enrollment, high dropout rates, and a startling lack of diverse representation, Jumo Health’s solutions aim to remedy these critical industry problems. Jumo Health’s curriculum-based educational solutions ensure prospective clinical trial participants have information relevant to their age, gender, race, language, and socioeconomic status at every stage of their journey, from pre-consent trial awareness to ongoing trial engagement. The result is faster recruitment, longer retention, increased patient compliance, and greater overall trial success for sponsors.
The Falfurrias investment will bring new resources and expertise to the Jumo Health team, aimed at expanding the organization’s core capabilities, enabling data-driven solutions, and widening patient engagement. Specifically, Falfurrias is energized by Jumo Health’s commitment to improving access to clinical trials among traditionally underrepresented communities, many of whom have a deep-seated mistrust of the healthcare system due to
historical inequities. Jumo Health has taken tangible steps to rebuild this trust by creating culturally sensitive materials and establishing a robust network of patient advocacy groups and more than 2,000 religious, social, government, and community-based organizations.
Adam Cossman, an executive advisor on the Falfurrias team with 25 years of pharmaceutical commercialization experience, will join Jumo’s board of directors as Chairman. Alexander Jutkowitz, an executive in residence at Falfurrias and global content marketing and communications expert, and Jackie Kent, a pharmaceutical executive with nearly 30 years of clinical trial innovation experience, will also join the board of directors.
“Treatment advancements for increasingly targeted patient populations depend on more diverse and innovative clinical trial solutions,” said Adam Cossman. “As treatments become more personalized and trial complexity increases, the need for effective patient communications is more critical than ever. Jumo Health’s patient-centric approach gets to the heart of these issues, and we look forward to helping them work towards their mission.”
“Since its inception, Jumo Health has differentiated itself by embracing storytelling as a means to increase health literacy across disparate groups, ensuring patients can understand their journey thanks to those that came before them,” said Kevin Aniskovich, President and CEO of Jumo Health. “This investment will provide the requisite industry expertise to speed product development, expand key customer relationships, and usher in a new way of thinking about access and ongoing patient participation in clinical research.”
“The Falfurrias team sees great potential in the clinical trial space,” said Geordie Pierson, Partner at Falfurrias. “It’s an area in need of tremendous attention. There’s a real opportunity to leverage Jumo Health’s foundational core in health literacy and expand its capabilities to form a broader, content-driven clinical trial offering that better serves
patients, doctors, and researchers alike.”
Equity for this investment comes from Falfurrias Capital Partners V, an operationally focused lower middle market buyout fund, and builds on the firm’s experience in marketing and communications.
Houlihan Lokey represented Falfurrias in this transaction, and Holland & Knight served as legal advisors. Jumo Health was represented by Canaccord Genuity LLC throughout this process.
About Falfurrias
Falfurrias Capital Partners is an operationally focused middle-market private equity fund focused on investing in high-growth companies in the food manufacturing, industrial technology, and business services sectors. The team is comprised of investors and proven operators, as well as in-house resources across strategy & market insights, finance & integration, human capital, and technology. The fund is managed by Falfurrias Management Partners, a Charlotte-based private equity firm founded in 2006 by Hugh McColl Jr., former chairman and CEO of Bank of America; Marc Oken, former CFO of Bank of America; and Managing Partner Ed McMahan. The firm has raised $2.2 billion across six funds and invests in growing, middle-market businesses in sectors where the firm’s operational resources,
relationships, and sector expertise can be employed to complement portfolio company executive teams in support of growth objectives. For more information, visit www.falfurrias.com.
Falfurrias Media Contact:
Steven Hirsch
Hirsch Leatherwood
[email protected]
The Importance of Prioritizing Self-Care for Parents of Children with Disabilities
Jumo Health has been the premier Champion Sponsor at the International Children’s Advisory Network (iCAN) Annual Summit for the last three years. This incredible event unites families and healthcare professionals worldwide for a week of sharing stories and ideas aimed at enhancing the global understanding of pediatric patients and their needs.
At this year’s summit in Italy, we had the privilege of meeting Michelle Burgess, a passionate advocate for patient-centric care. Michelle’s mission is to support parents of children with disabilities and emphasize the critical importance of self-care. She shared her journey, underscoring how parents often neglect their well-being while caring for their children, leaving both the parent and child vulnerable.
Michelle’s story is particularly profound. In 2008, just four days after the birth of her fourth child, Michael, she and her husband were told their newborn son had sickle cell disease. After diagnosis Michelle and her husband engaged with doctors and read extensively about sickle cell in order to become well-informed regarding their son’s condition. Then, in 2022, when Michael was 14 years old, Michelle was rushed to the hospital in critical condition, fighting for her life. A sepsis infection had gone untreated, sending her into septic shock and causing her heart and kidneys to fail. At the same time, her husband was being asked if she had a DNR (do-not-resuscitate order); their son, Michael, was experiencing a severe sickle cell crisis that put him in the hospital as well. Yet, despite these overwhelming challenges, Michelle and her husband managed to focus on both her recovery and Michael’s care.
“I think parents that have children who are living with disabilities and challenges, we put ourselves on the back burner because we’re trying to be there for them. Ultimately, that is the worst thing you can do because you are making yourself vulnerable and that child vulnerable if you do not support and care for yourself.”
While talking with Michelle, she highlighted the crucial need for parents to seek support and prioritize their well-being to care for their children effectively. She also addressed the complex decision they faced regarding clinical trials for Michael, noting her initial fears because of the historical harm done to the African American community through clinical trials. However, faced with Michael’s increasingly low hemoglobin, they chose to enroll him in a trial, which led to significant improvements in his health.
Michelle’s advocacy now focuses on educating parents about the importance of clinical trials and improving diversity within them. We are incredibly grateful to have heard her story firsthand.
Building Tomorrow’s Healthcare: The Vital Role of Young Voices in Medical Communications
Jumo Health, a global provider of age-appropriate, culturally relevant medical education resources, is proud to celebrate International Youth Day by reflecting on the invaluable insights gained from young people around the world. Our long-standing partnership with the iCAN (International Children’s Advisory Network) Summit, where we have been the lead sponsor for the past six years, has continually shaped and guided our mission. The iCAN Summit is more than just an annual event; it is a vibrant, living testament to the power and importance of youth voices in healthcare.
This year’s iCAN Summit, held in Bari, Italy, provided a unique platform for children and young adults, many of whom live with chronic conditions or rare diseases, to engage directly with medical professionals, community leaders, and advocates. Listening to their stories, challenges, and aspirations is not only an inspiration but also a critical component of our work at Jumo Health. The insights we gather from these young participants ensure that our medical communications are not only theoretically sound but also practically relevant and deeply empathetic.
One of the primary focuses at this year’s summit was improving the clinical trial Consent/Assent process. Through interactive sessions, we explored how different media—such as video, animation, and personal discussion guides—affect comprehension and engagement. The clear preference for video and in-person discussions reaffirmed our commitment to using these mediums in our products. This commitment is driven by the understanding that young people learn best when the information is presented in ways that resonate with their experiences and preferences.
The power of storytelling and the theme of self-advocacy emerged as central pillars during the summit, highlighting the profound impact that sharing personal experiences can have on understanding and navigating complex medical information. Hearing the stories of other children not only made participants feel less alone but also empowered them to take charge of their health. This realization continues to drive our efforts at Jumo Health to create relatable, story-driven content that resonates with young audiences.

During the summit, we had the privilege of capturing over 20 personal stories from young people and adults, which have already been developed into compelling videos to be shared across multiple online platforms. By incorporating these real-life experiences into our educational materials, we make complex medical concepts more accessible and relatable, while also fostering the self-advocacy that is crucial for young people to become active participants in their healthcare journeys. This approach ensures that the next generation is equipped with the knowledge and confidence they need to make informed decisions about their health.
Another critical insight from the summit was the importance of building digital trust. In a session focused on this topic, both parents and children emphasized the need for transparency and trustworthiness in online medical information. This feedback has helped us refine our digital strategies, ensuring that our content not only educates but also builds trust with the families who rely on it. In today’s digital age, trust is paramount, and we are committed to maintaining the highest standards of integrity and transparency in all our communications.
Our time at iCAN serves as a constant reminder of the importance of centering young people in everything we do. Their insights shape our strategies, influence our product development, and ultimately help us create better health outcomes for all. As we reflect on International Youth Day, we are more committed than ever to continuing this vital work, inspired by the incredible young voices we are privileged to hear at iCAN. Together, we are building a brighter future for healthcare—one where young people are not only heard but also empowered to lead the way.