A Discussion on Innovation in Clinical Trials
Jumo Health Participates in a Tweet Chat with Experts in the Industry
Today is International Clinical Trials Day. To celebrate, we participated in a tweet chat with our friends at Eli Lilly and other experts in the industry about how innovation is taking hold in clinical trials. The conversation focused on how innovation should be centered on the patient and the importance of practical solutions that solve for the core issues. Read below for some of our thoughts on the topic in 280 characters or less…
Question 1: How would you define “innovation” when it comes to clinical trials?
Thought #1: Innovation is intended to ease a burden or solve a problem. Jumo Health innovates by providing solutions that work the way people live. We do this to ensure mass appeal and broad utilization. Without this, innovation is simply fodder for textbooks.
Thought #2: All innovation in clinical trials should be centered around the patient. While some may think AI, at Jumo Health, we address core issues that prevent optimal outcomes and focus on age appropriate resources to overcome health literacy challenges.
Thought #3: A practical approach to innovation matters because the stats don’t lie. ~85% of all clinical trials experience delays. 50% of adults can’t read above an 8th grade level, and non-compliance hovers ~70%. Innovation should focus on the root cause.
Thought #4: Our definition of innovation is embodied in our product design and through a range of age appropriate offerings from comic books to animations — all of which are intended to allow patients to understand and act upon their health care instructions.
Question 2: What recent innovations have you seen that have created a more patient-centric clinical trial experience?
Thought #1: The paradigm shift of placing patients at the center of product design is finally taking hold in clinical trials. Will this innovation make an impact on increasing health literacy? If so, then achieving optimal outcomes and compliance is right behind.
Thought #2: The informed consent process is broken. We love when organizations take steps to produce materials that augment the med-legal requirements with patient-friendly, engaging, and actionable resources.
Thought #3: We applaud organizations that take a patient-first approach. Our friends at Eli Lilly used mixed media resources, tailored for each age cohort, to break down complex medical information and make the unknown less scary. Check it out here.
Question 3: CISCRP’s 2019 Perceptions and Insights Study found that technology is playing an increasingly larger role in clinical trials. What technology do you think has been the most impactful for the patient experience?
Thought #1: Even though the study was fielded before the COVID-19 pandemic, the future role of tech in patient-centered health care is tricky due to HIPAA and GDPR, and further complicated by those who are traditionally underserved without access to certain tech.
Thought #2: ePRO, eCOA, and telemedicine solutions have taken positive steps in the space to help increase access and ease the day to day. The platforms also require best in class educational resources to become a stronghold.
Thought #3: Virtual reality is just starting to play a role. Long study visits often increase the patient’s fear and anxiety. The immersive experiences provided help calm and distract participants while supporting overall well-being.
Question 4: How can innovation lower barriers to participation in clinical trials?
Thought #1: Innovation is not a panacea. Fundamental educational deficiencies plague the health care industry. To push clinical trials forward using tech such as IBM Watson, we need to ensure patient-friendly materials are at the forefront of the experience.
Thought #2: Allow for a patient-friendly informed consent experience. Period. As study protocols become more complex, the onus is on us to ensure patients and caregivers can understand what is being asked of them. This upfront step will reduce dropout.
Thought #3: Informed consents are typically written at an 11th grade reading level; yet 50% of adults can’t read above an 8th grade reading level. 35% of people who dropped out of a clinical trial found the informed consent difficult to understand.
Thought #4: Businesses that reach out to the community physicians to ensure those traditionally underserved can benefit from novel approaches to treatment such as Elligo Health.
Thought #5: Mixed media resources that are available in the community will ensure that every patient, regardless of educational attainment or socio-economic status, can understand, manage, and own their own health.
Question 5: What is an innovation that you’re hoping to see in clinical trials in the near future?
Thought #1: Enterprise tech such as IBM Watson shows promise but in order to more effectively impact patient care and outcomes, we are bullish on basic building blocks such as data analytics to identify key inflection points and customer service platforms.
Thought #2: Wearable devices that can help track a participant’s progress, send reminders and positive notes, and allow for easier communication between participants and site staff.
Thought #3: Customer service platforms! Treat a participant like a consumer. Innovation doesn’t need to re-invent the wheel — it often just needs to apply decades of learnings to health care.
Thought #4: Actionable patient resources! We are committed to solving the fundamental challenge that plagues the point of care by delivering patient-friendly, evidence-based, and peer reviewed resources.
Thought #5: A greater focus on pediatric trials both related to the RACE Act and among all disease types.
Thought #6: Expanded health literacy! We see a future where the statistic that 90% of the population are health literate — acting upon their physicians instructions to meet their end goals.
Thought #7: Solutions that bridge relationships between patients, the site staff, and the larger clinical trial community. Patients want a sense of connection and to be appreciated for their participation.
We Are Jumo Health: Columba Quigley, MD
An Interview with Editor in Chief, Columba Quigley, MD
Great companies are made up of great people. Here at Jumo Health, our most valuable resource is our team. We are a collective of medical folk, product people, designers, and storytellers that share a common goal to change health care today. Through our We Are Jumo Health series, we will introduce you to the dedicated people who are the heartbeat of Jumo Health.
This month, we’d like you to meet Columba Quigley, MD, Editor in Chief of Jumo Health. Columba has been a member of our team for nine years. Her expertise and wisdom has proven invaluable not only to the work we create, but also to her colleagues who seek her guidance. Meet Columba!

What led you to Jumo Health?
My background is in medicine and I worked as a hospital-based physician for many years. Over that time, I became increasingly interested in the language of medicine, in how we communicate stories of illness, and also the gap that seems to exist between “medical jargon” and a patient’s understanding. Initially, I studied the language of illness from an academic perspective, becoming a humanities scholar in the field. One of the areas I was specifically interested in was the world of graphic medicine — the power of that specific visual and verbal format to uniquely communicate stories of illness.
What is your favorite part about working at Jumo Health?
What we achieve: making the confusing less so for a potentially vulnerable audience; who I work with: an amazing team that is both creative and compassionate, and fueled by a similar passion.

What motivates you?
The belief that I might be helping those who are ill and at the same time confused and anxious about their medical condition and what they might be facing. Also, I believe that “knowledge is power” and if we can help people understand their illness and why they need to comply with prescribed treatment regimes, then their clinical outcome may actually significantly improve.
What is your proudest achievement at Jumo Health?
Increased focus on health literacy. By working to ensure that our resources are truly literacy sensitive and truly accessible to and understandable by our target audience.
What are you most excited about for the future of Jumo Health?
Having witnessed the company achieve so much over the past years, I am really excited about its potential to realize even more achievements in the health care space.
If you could do any other job for one day, what would it be and why?
Be a concert pianist. Because it might transport even one audience member to a place of (albeit transient) sublime joy.
What is the most important thing you’ve learned in the last five years?
Humility.
Finish this sentence, I am happiest when…
I happen upon random and unexpected moments of joy.
If you want to learn more about Columba, you can connect with her on LinkedIn. Want to work for Jumo Health? Check out our career opportunities!
What is a Virus? Our Resource Helps Explain
During this trying time for our global community, it’s safe to say one word on everyone’s mind is “virus.” But, where to turn for safe, reliable information that you don’t need a white coat to understand can sometimes be difficult.
At Jumo Health, we create highly visual resources based on the latest medical research using storytelling to explain difficult medical concepts. With such an influx of information being relayed from all directions surrounding the coronavirus and COVID-19, it can be helpful to take a step back and start at the beginning. We have a number of resources relevant to the current pandemic.
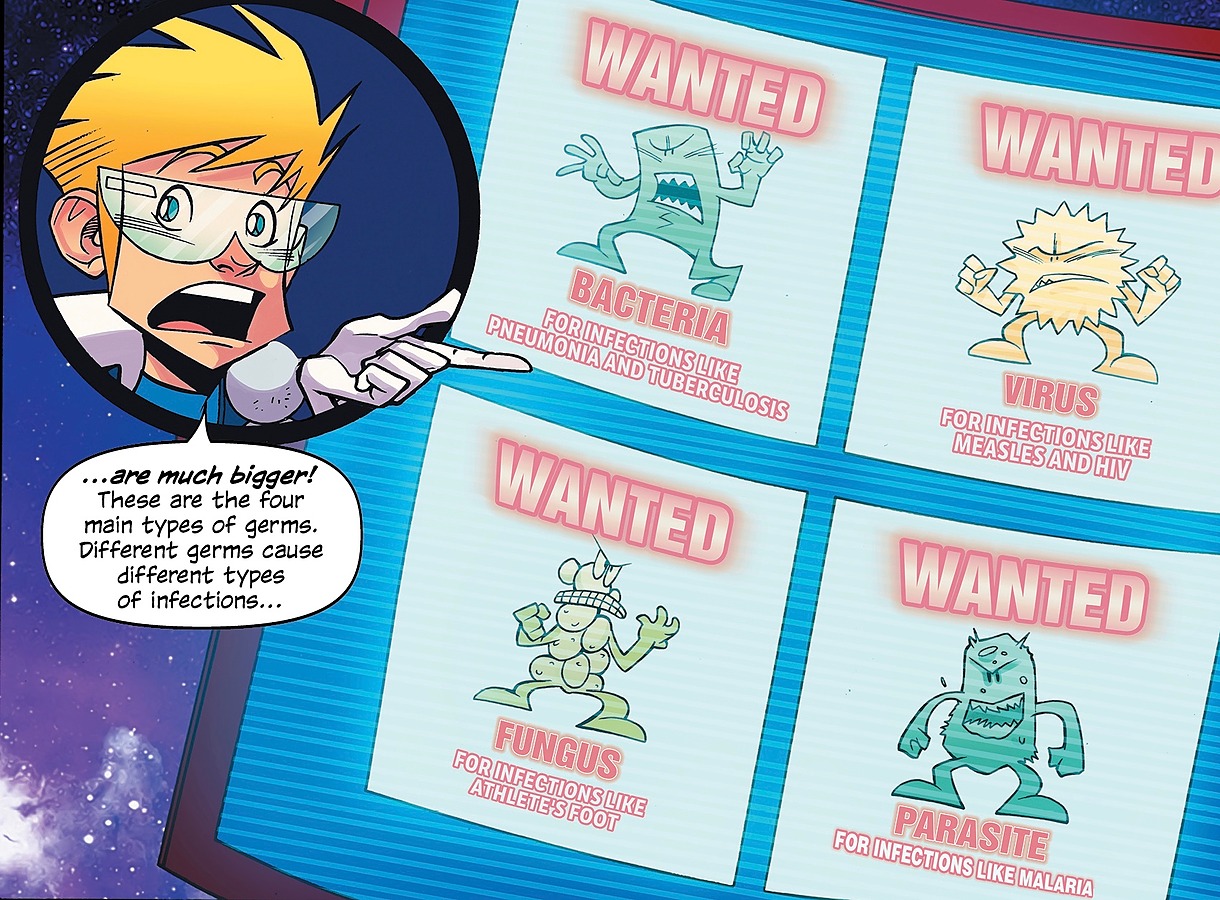
To start with, our title on infections addresses a key question that may not be the first to come to mind, but is particularly relevant: what is a virus?
It can be difficult answering even this simple question for kids. Understanding Infections addresses this difficulty by creating an engaging adventure story around the medical facts, in a language and style that engages and entertains while simultaneously educating. As the fictional “Mediland” becomes “invaded” by germs (a narrative that resonates with what the world is currently experiencing) two of the resident superheros (the “Medikidz”), Axon and Abacus, explain what infections are and the different types of causative germs, including the type on everyone’s minds.
As the story continues, the Medikidz proceed to explain various types of infections, from the common cold to more serious conditions, such as meningitis. How infections can be treated and prevented is also explained.
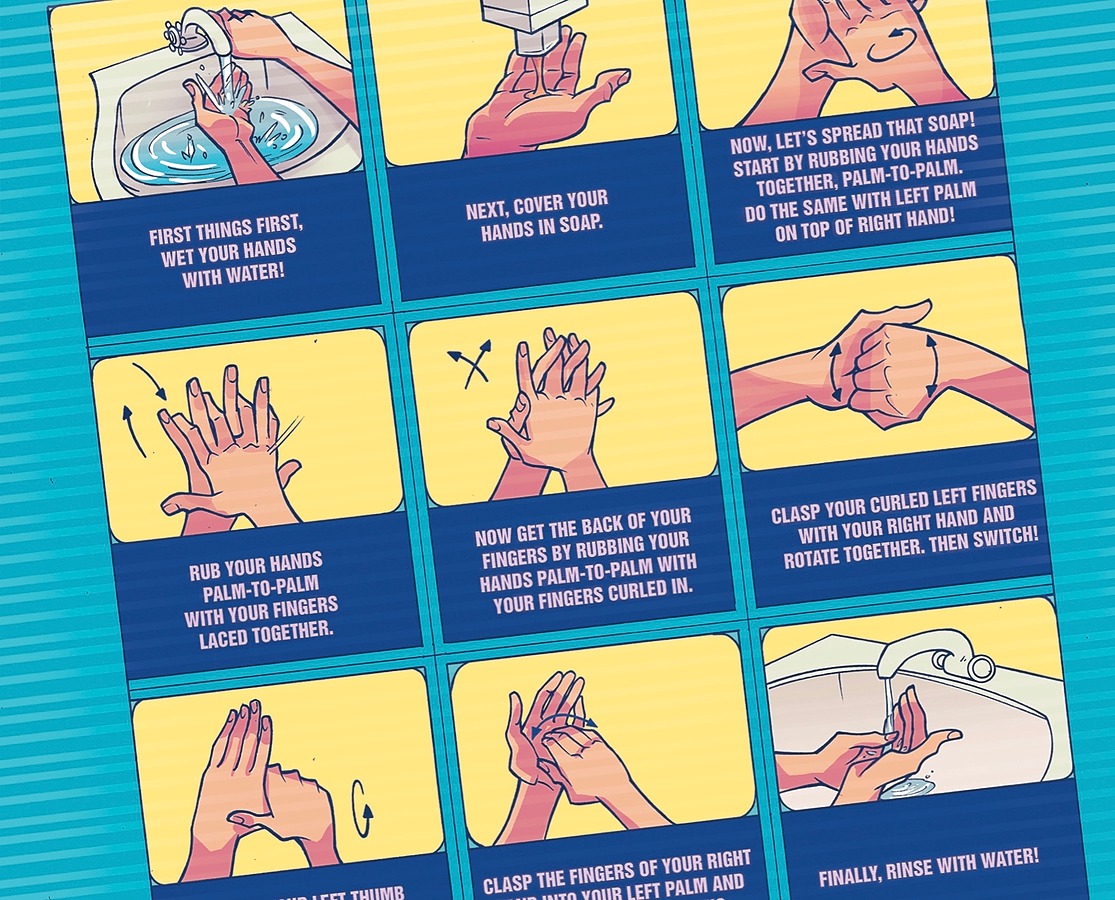
The book ends with the most important message of all— the best way to prevent infections is through regular and thorough handwashing. The current pandemic has highlighted the fact that how we have been washing our hands to date generally falls well short in terms of preventing the spread of disease. Understanding Infections includes a full page visual step-by-step guide on how we should be doing this critical infection prevention measure.
Understanding Infections answers simple questions that our young audience ask and can relate to. Arming oneself with facts and thereby influencing health behavior is very much at the core of the Jumo Health ethos.
Read our Understanding Infections book here!
A Letter Concerning COVID-19
Dear Friends,
Like all other companies, Jumo Health is actively monitoring the COVID-19 situation. As a global organization, we are keen to protect our employees, their families, and our business commitments to clients and their patients during this time of uncertainty.
On March 10, 2020, we activated our business continuity plan (the “Plan”) which places into practice standard operating procedures during times such as this. The purpose of the Plan is to:
- protect our employees and the broader community,
- mitigate the anxiety often associated with the unknown, and
- maximize productivity and minimize disruption for our clients
Ensuring that our employees work from a space where they feel safe permits us to collectively serve our clients and their on-going needs without interruption. Our Company is used to working across time zones and in remote situations with team members and clients alike. Our secure video conferencing capabilities, HIPAA-compliant cloud storage systems, and adaptive culture allow us to provide the same value and work ethic today that led you to select us to serve your business needs previously.
To Our Clients
We have planned for such an occasion. Our supply chain is intact and our production teams are fully operational. We are prepared and positioned to weather this storm with you.
Our agile response system allows us to produce the most pressing resources as efficiently as if we were all in the same building. For those with current projects, we appreciate your continued commitment to the patients and their care circle that require your services. We agree that it is prudent to persevere through this trying time to ensure we are ready without delay when we can successfully flatten the curve.
While no one could have guessed that a coronavirus would lead to our business continuity plan being successfully activated and managed, we are grateful that all team members in the United States, England, South Africa, Italy, and New Zealand are safely working from home without any disruption in productivity.
As always, we remain at your disposal.
Being Present in our Communities
Being a good corporate citizen has taken new meaning here at Jumo Health. Our strength is our people. From donating meals to local food banks and soup kitchens, to organizing grassroots campaigns to donate personal protective equipment like masks, our people have stepped up to play their role in serving our communities.
In addition to our employee contributions, Jumo Health will be providing newly released COVID-19, hygiene, and other related resources to hundreds of hospitals at no cost.
Looking Forward
The COVID-19 pandemic has presented us with a challenge we all endeavor to overcome. As the situation continues to unfold, we are reminded to be grateful for the allied health professionals who show up each day to treat the sick, for those working at pharmacies who keep needed medications readily available, to restaurants and grocery stores that keep us fed, and the countless others that place the many before themselves.
While the unknown continues to outpace that which we know with any certainty, the Jumo Health family remains confident in our resolve as a people, bullish on our industry’s ability to self correct, and excited to see this new normal shape our future.
Jumo Health is here today and ready for tomorrow. Stay safe and healthy and let us know how we can help.
Thank you for your continued trust and support.
Kevin Aniskovich
President & CEO
Patient Experience: Benefits, Strategies, and FAQs
What Is Patient Experience?
Patient experience comprises all of the ways that a patient interacts with a medical provider. Both positive and negative experiences with doctors, nurses, office staff, administrators, clinical trial professionals, insurance agents, and even pharmaceutical representatives shape the patient’s overall attitude and affect health outcomes.
In order to provide high-quality, patient-centered care, it is important to cultivate an end-to-end patient experience focused on putting the patient’s needs first. We’ve put together some ideas on how medical professionals can improve patient experience in their practice.
Defining Patient Experience
Patient experience encompasses all the ways that patients connect with their health care providers. Obvious examples include formal communication with medical staff, pharmacists, office workers, and administrators. Less obvious examples might include things like making sure the facility is accessible, especially during times of construction or maintenance, and preventing potentially negative encounters, such as making sure employees who smoke do not do so near the medical facility. Regularly reviewing behaviors, habits, policies, procedures, technology, and premises from the patient’s point of view will help to ensure a positive and inclusive experience.
Note that patient experience also includes the entire care circle’s experience. Patients who are unable to attend to their own medical needs – e.g., those who are young, severely ill, or have a disability – may have family members who help them with accessing medical care. It is just as important to consider the experience of engaged family members and other supporters as it is the patients themselves.
Patient Experience vs. Patient Satisfaction
Patient experience and patient satisfaction are often confused. A patient’s experience can affect the level of satisfaction, but satisfaction can also be affected by a patient’s expectations. Managing those expectations is part of the overall patient experience, and doing so effectively will often lead to higher rates of satisfaction.
Measuring patient satisfaction is not enough in itself in terms of enhancing our understanding of how to improve the patient experience. It is important to ask both qualitative and quantitative questions when requesting feedback from patients. Such feedback may not always be easy to obtain, so offering multiple ways for patients to supply comments about their experience is best. Real-time feedback has as much of a role as satisfaction surveys that may be sent out later.
5 Ways to Improve Patient Experience
There are many factors that affect patient experience, some of which may be unique to the health organization’s people and operations. At a high level, however, the following factors are some of the most important ones to consider when working to improve or maintain a positive patient experience.
1. Foster A Caring Culture
Organizational culture plays a significant role in patient experience. Culture relates to how the organization operates, including everything from the day-to-day tasks of those who oversee a patient’s care plan to the high-level decision-making process of executives or others in leadership roles. Health care organizations that focus more on the bottom line than on the experience of care will have a hard time making significant improvements.
Rethinking a health care organization’s culture – and the patient experience – can happen at any level, and organizations that encourage innovation and creative improvements will most likely experience the best benefits for their patients. Some organizations are even hiring “Chief Experience Officers” to help shift their culture to a more patient-centered approach.
2. Communicate Better With Patients
Patient communication is more complicated today than ever before. In addition to face-to-face conversations with doctors and office staff, patients may receive emails, phone calls, texts, app-based information, and even good, old-fashioned snail mail. The communication choices currently available are incredible, but they can also negatively impact the patient experience if they are not used appropriately.
Communication is important because it helps maintain a continuum of care. Some patients may only want their medical provider to send them appointment reminders and bills. Others will appreciate a wider variety of communications that provide helpful information about their own medical issues or other health concerns they may be facing. Offering communication options that meet the needs of a diverse patient population – and making it easy to find and update those options – will help improve the patient experience.
When looking at communication options, be sure to consider innovative patient education materials like comic books, videos, and podcasts to help patients understand the nature of an illness, procedure, medication, and other health topics.
3. Connect with Patients on a Human Level
Connecting with patients on a human level is a critical component of care delivery – even when those connections have nothing to do with medical care itself. Patients will generally have a more positive experience if they have a good rapport with their doctors, nurses, and other staff.
Making a human connection can happen during any interaction, from making appointments to having conversations about whether a patient will be able to pay an unexpectedly large bill. Finding a way to show genuine interest in patients as people lets them know they are valued. First points of contact are critical, but ensuring end-to-end communication with patients at every stage in their journey is just as important.
4. Address Patient Expectations
A remarkable amount of the patient experience is driven by expectations about their care. Studies have shown that quality of life is affected significantly by the gap between patient expectations and the actual care experience, and different expectations can lead to different views about their quality of life – resulting in different experiences for patients despite receiving the same care.
Setting patient expectations about their care up front can lead to a much better experience. While it is good to give patients hope and encouragement, medical providers should not over-promise or imply that a patient’s outlook is better than it really is. Likewise, when dealing with administrative or billing issues, expectations should be set up front, so that patients understand what to expect in terms of payments, insurance submissions, and related activities.
5. Ask for Feedback
Perception is related to expectation in that it requires tailoring communications to make sure patients understand exactly the type of care they receive (or are going to receive). Patients who believe they are receiving one type of care, only to receive another, may be confused, angry, and feel like the quality of care is not as good as it should be.
Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys can also improve the patient experience by giving health systems important information about how patients think they are doing. Hospitals and other medical centers should use HCAHPS feedback to make quality improvements that will benefit the patient experience.
Benefits of Improved Patient Experience
Why should medical providers worry about the patient experience? Here are a few of the reasons why we should make the patient experience a priority.
1. Improved Patient Safety and Clinical Outcomes
A review published in BMJ Open looked at evidence from 55 studies to better understand the relationship between patient experience, patient safety, and clinical outcomes. The authors of the review concluded that there is indeed a positive relationship between these three factors, and that a reduction in focus on the patient experience could actually result in a reduction in patient safety, as well as having a negative effect on clinical outcomes.
2. Less Utilization of Unnecessary Health Care
Overtreatment is a growing problem, some of the reasons for which can be attributed to poor patient experience. Patients who believe they did not receive the right type or quality of care may often seek additional care, which may not be needed and could even be harmful, depending on their medical situation. At least some patients who report a positive experience have lower readmission rates, depending on the severity of their disease.
3. A Better Relationship With Disease
Finally, from the patient perspective, a positive experience can help patients better cope with the realities of the medical issues they are facing. Particularly for those facing a poor prognosis, positive patient experiences can lead to a better quality of life by helping the individual focus on supportive or palliative care, rather than on negative experiences with their medical provider.
Health Literacy: What It Is and How to Improve It
What Is Health Literacy?
Health literacy is the ability to access, understand, and act on information that affects one’s health. While literacy refers to the ability to read and write, health literacy is more complex. Many internal and external factors are at play, for instance, a person’s math skills and a healthcare provider’s cultural background. And while literacy informs a person’s ability to be successful in school or at work, health literacy can have life-or-death consequences.
In addition, the economic toll of poor health literacy is between $108 and $328 billion per year. To put this in perspective, the potential savings of improved health literacy matches the cost of providing healthcare coverage to the nearly 50 million Americans who were uninsured in 2006 (based on U.S. Census Bureau estimates). When the future implications of poor health literacy are considered, this cost is predicted to compound to between $1.6 and $3.6 trillion.
Why Health Literacy Is Important
Well-informed patients naturally feel more confident interacting with healthcare professionals and making medical decisions. Studies also suggest that patients with poor health literacy have worse medical outcomes. Broadly speaking, poor health literacy impacts adherence and compliance to medication. In clinical trials, poor health literacy impacts recruitment and retention.
Poor health literacy is also associated with decreased preventive care and increased use of emergency medical services, which are not only more costly to the patient and the healthcare system as a whole, but also reduce a patient’s chances of positive treatment outcomes due to delayed intervention. For instance, if a patient puts off seeing his/her doctor for a cough that turns out to be lung cancer, the prognosis is likely to be worse, and treatment options more limited, than a patient who had visited his/her doctor soon after symptoms arose.
Put simply, proficient health literacy puts the patient in the driver’s seat, resulting in more consistent, compliant, and effective healthcare for the patient—and also one that is more cost-efficient.
Factors that Affect Health Literacy
Health literacy depends on a complex matrix of factors, including:
- General communication skills
- Cognitive abilities
- Learning abilities
- Educational opportunities
- Culture
- Cultural beliefs
- Values
- Traditions
- Attitudes toward medicine
- Language
- Written literacy
- Digital literacy
- Visual literacy
- Computational literacy
Depending on the situation (e.g., the patient/healthcare provider’s relationship or the environment), different combinations of these factors can come into play. For instance, a patient who shares the same cultural background as his/her healthcare provider may feel more comfortable and have an easier time communicating because they share not only the same language or dialect but also hold the same cultural beliefs and values.
5 Ways to Improve Health Literacy
Because health literacy is a systemic problem, the onus of improving it does not fall on the patient. Healthcare providers and institutions must work to better educate patients, meet them on their level, and ensure medical options, instructions, and treatment plans are fully understood. The following are some of the ways healthcare providers can improve the health literacy of their patients and their caregivers.
1. Improve Patient Educational Materials
Patient education is a collective term for the process in which doctors, nurses, and other healthcare professionals pass on information to their patients and their families or caregivers. The effectiveness of this process can have long-term impacts on patients’ health, both positive and negative.
Today, this information transfer can take place in a variety of ways—from the traditional pamphlets you see in waiting rooms to podcasts, videos, and even comic books. Whatever the method, the most important thing for healthcare professionals to remember when selecting resources for their patients is to meet them on their level. For instance, educational materials for children should be engaging, relatable, and visually compelling. When patients are able to connect with educational materials in a more meaningful way, they are better able to receive and retain the often complicated information being imparted to them.
Check out Jumo Health’s collection of age-appropriate educational materials.
2. Provide Regular Staff Education
To improve patient education, and consequently health literacy, medical staff must be trained in best practices for delivering educational material. Therefore, all staff should receive regular, standardized training on how to best educate patients.
3. Use Plain Language When Communicating With Patients
Plain language refers to communication that can be understood by the recipient the first time it’s presented. Using plain language is one way healthcare providers can help improve health literacy. By using clear terminology, patients have a much better chance of understanding their condition, options, treatment plan, and doctor’s instructions. Plain language can also help break down other potential barriers to communication, like the sense of inferiority that comes with feeling like you’re being talked down to. This is true of both conversational and written communication.
It’s also important to note that what is considered to be plain language to one person may not be to another. For this reason, testing your plain language communication with patients can help determine where gaps may still exist and where adjustments may need to be made (on a person-by-person or community basis).
When used effectively, plain language can go a long way toward satisfying the main components of health literacy: enabling the patient to better access, understand, and act on the (often) complicated information being presented to them. Some of the ways healthcare providers can incorporate plain language practices into their communication include:
- Using active voice as much as possible
- Using a hierarchical approach (starting with the most important information)
- Avoiding jargon
- Taking time to break down complicated topics and terminology
Along with using plain language as a best practice, healthcare providers should also be sure to clearly spell out the basics: what, why, when, and how. For instance, when antibiotics are prescribed, it’s important that a healthcare provider explains the purpose of the drug and how it will affect the patient’s condition, why it must be taken twice per day for the duration of the prescription (and the consequences of not doing so), and how it should be taken with food to prevent nausea. It can be easy for healthcare providers to gloss over these seemingly small, but important details after having prescribed the same medication hundreds of times over the years.
4. Demonstrate Cultural Competency
Because culture plays a large role in how people communicate, healthcare providers must pay special attention to how they transmit information to patients with different cultural backgrounds. As mentioned above, differences in a patient and their healthcare provider’s cultural beliefs, values, traditions, and attitudes toward medicine—and, of course, language—can all be barriers to effective communication.
When healthcare providers address patients of different cultural backgrounds in a respectful and culturally relevant manner, there is a much better chance the patient will hear and retain the crucial information being conveyed. In addition to being conscientious of how patients are addressed, there are many resources available to healthcare providers who want to become more culturally competent. This investment can make a noticeable difference in treatment outcomes.
In terms of language, the National Standards for Culturally and Linguistically Appropriate Services in Health Care recommends that healthcare providers offer language assistance services at no cost to the patient. In fact, most states (as well as Title VI of the Civil Rights Act of 1964) now require this. While it’s ideal for medical offices to have bilingual employees on staff, translation services and interpreters can also help bridge communication gaps for patients with limited English proficiency. The standards report also advocates for having educational and print materials available in languages that are common to regional populations.
5. Request Patient Feedback
Despite healthcare professionals’ sound intentions of accurately communicating medical information, the intricacies of the message can easily be lost in translation. For instance, a patient with proficient health literacy skills receiving a life-changing diagnosis from their doctor may not fully process the conversation or retain some of the more crucial details. The emotional impact of the diagnosis may temporarily affect the patient’s ability to process information, and some important details of the condition may not be received and understood as intended.
This is where feedback comes in. Soliciting patient feedback is a solid way of not only assessing health literacy but also ensuring the information given matches the information received by the patient. This feedback could come through a variety of methods, which should be used in tandem for best results, including:
- Asking a patient to repeat information back to you (also referred to as the “teach-back” method)
- Allowing time for questions and answers at the end of an office visit
- Following up with a phone call after a visit
- Administering patient experience surveys
Low Health Literacy: Who is at Risk?
While there is a correlation between literacy and health literacy, no one is immune from health literacy challenges. Only 12% of American adults are considered proficient in health literacy and more than a third have only “basic” or “below basic” health literacy levels. This equates to nearly 80 million Americans who have trouble following simple medical instructions provided by their medical professional or making the appropriate determinations on whether treatment should be sought, for example.
The following are some of the populations most at risk of health literacy challenges:
- Older adults
- Minority populations
- Uninsured populations
- Low-income populations
- Populations with limited education
- Populations with limited or no English proficiency
- Immigrant and refugee populations
Older Adults
Adults 65 years of age or older have been shown to have lower health literacy levels than those under 65. This disparity is most striking for the 75-and-over group, with more than two-thirds of adults showing basic or below basic health literacy skills.
Minority Populations
While adults in any racial and ethnic group can have basic or below basic health literacy, white/Caucasion adults represent the smallest portion (28%) in these categories. By contrast, 66% of Hispanic adults have basic or below basic health literacy skills, and black/African-American adults have 57%. When the below basic category is considered on its own, 41% of white/Caucasion adults and 35% of Hispanic adults make up this designation.
Uninsured Populations
The uninsured and those with Medicaid or Medicare are four times more likely to have below basic health literacy skills than those with employer-provided insurance. For those with employer-provided insurance, the proportion of adults with basic or below basic health literacy is approximately one-fourth, whereas more than half of the uninsured population and those with Medicaid or Medicare make up these groups.
Low-Income Populations
Lower incomes are also associated with poor health literacy. Those living below, at, or just above the poverty level have an average health literacy in the basic range, compared to intermediate (just below proficient) for those whose income is at least 175% of the poverty level.
Populations with Limited Education
Education and health literacy are closely linked. For instance, only 1% of those with less than a high school education are considered proficient in health literacy, compared to 30% of those with a bachelor’s degree. The story is even more telling for the group with below basic health literacy; 49% of those with less than a high school degree and just 3% of those with a college degree fall into this category.
Populations with Limited or No English Proficiency
Because English proficiency is a prerequisite for health literacy in America, populations with limited or no English language skills are at increased risk of having poor health literacy.
Immigrant and Refugee Populations
The American healthcare system is complex and can be difficult to navigate for those who were born here, let alone those who were not. For immigrants and refugees coming from other countries with entirely different healthcare services, practices, and insurance systems, it can be overwhelmingly complicated.
Damon: A Real Life Osteosarcoma Hero
“Strength isn’t how much one can lift. Strength is how much one can lift others!” – Damon Billeck
Meeting Damon For the First Time
The first time we met Damon, he was on his way to present the Courage Award at the Sarcoma Foundation of America’s Annual Gala, an award that he had received the previous year. Dressed in a tux with a yellow vest and bow tie – the color of sarcoma awareness – we were thrilled to meet the star of our Understanding Osteosarcoma comic book. Everything about him was inspirational, particularly his sunny disposition and eagerness to help others no matter how he was feeling. Whether recording a video with words of encouragement for others battling cancer, or delivering gifts to those in the hospital over the holidays, his desire to help others was evident in everything he did. Sharing his story with the world through our Understanding Osteosarcoma comic, in the hope that it would ease the fears others may have when diagnosed speak to this giant of human being.
The Importance of Spreading Awareness and Sharing Your Story
Having a medical condition can seem isolating. Each day we try to bridge that gap by providing resources that engage and, through the experiences of others, inspire.
The story presents Damon as a superhero (we’ll get to why later) and includes members of his family as well. Both on and off the page, Damon was truly his twin sister Dara’s very own superhero. A lover of Captain America, Damon was diagnosed with osteosarcoma at age nine, and passed away this spring, four years later. Reflecting on Damon’s participation in creating the comic book, his father shared, “that was his crowning achievement, he loved carrying out his story and helping others get through it.”
Damon was a hero to many, including the “real” Captain America, Chris Evans. Damon shared his comic with Evans, because, as his father says, “Damon wanted his hero to see him as a hero.” And Captain America did not disappoint when he autographed Damon’s comic book and continued their support for one another on social media.
July is Sarcoma Awareness Month. We remember Damon as we continue to fulfill his hope that other children and their families might benefit from hearing and understanding his personal and courageous story.
Learn More about Damon’s Story, Osteosarcoma, and the Connection to Captain America Chris Evans
- Read the comic
- Watch Damon’s words of encouragement
- Sarcoma Foundation of America
- See Chris Evans’ tribute to Damon