Jumo Health: Working with Families
Since joining Jumo Health, I have been impressed by how much my colleagues know about the families that we feature in our content. They speak about families they have met as if they are friends.
Fast forward six months into the job, and I am traveling to go on my first patient filming, which features Vaughn Ripley.
Vaughn was diagnosed with hemophilia A when he was an infant. Hemophilia is a condition in which a person’s blood does not clot properly due to lack of clotting factor. This means that when a person is injured, a wound can bleed too much, which stopped him from participating in activities he was interested in, like baseball and football. As a teenager, after living with hemophilia A, he was diagnosed with HIV and hepatitis C, and was told he had less than 2 years to live. Vaughn openly talks about his struggles with depression and substance abuse, and credits his wife, Kristine, for being his partner through it all. Together, they were able to lift Vaughn out of his depression, and today they live a fulfilling life with their two kids and family pets.
I was anxiously awaiting my trip down to Maryland. I had seen an existing video of Vaughn, and this guy is charismatic. I wondered what he and his family would be like in person.
Vaughn brought himself, his wife, and two children to the filming. We met at a campsite where Vaughn and his family were able to hang out doing things they love to do, like swimming in the Potomac River, riding bikes on the nature path, and hanging out chatting at the picnic tables.
His family automatically made us feel comfortable. We were sharing sunscreen, bug spray, and popsicles. Fast forward a few hours and Vaughn is driving my colleague Becca and me around the campsite in his off-road Jeep, the kind without doors or a roof… there is never a dull moment!
The following day, we walked in with our film crew to Vaughn and his wife cooking us bacon and bullet proof coffee. After a few minutes, I forgot we had only met Vaughn and his family the day before. It felt completely natural to hang out, film, record podcasts, share meals, and play around with their pets in the house. What was even cooler was to hear Vaughn give his interviews. He speaks candidly about his conditions and how they have impacted his life, but he doesn’t let his diseases define him. As charismatic as he is on screen, he is equally as engaging in person. I was truly interested in every piece of his story that he shared with us.
After a quick piano concert performed by Vaughn’s daughter, Becca and I were ready to hit the road and drive back home.
We left Vaughn’s house that evening with a renewed sense of purpose, full of energy and ready to help share his story.
This is what makes working at Jumo Health so special. We feature real patients and are able to provide authentic content as a result. Now, I can honestly say that this was a family and an experience I’ll never forget.
Interested in joining the team and working with families like Vaughn’s to share their stories with the world? Check out our careers section.
We’re adding new content every day. Check out our Hemophilia Resources.
ADHD and Media Use
ADHD – Definition and Prevalence
Attention-deficit/hyperactivity disorder (ADHD) is a chronic condition characterized by persistent problems with maintaining attention, hyperactivity and impulsive behavior. ADHD affects millions of children – between 5% and 7% in the US – with reports suggesting that the prevalence is increasing. The exact cause of ADHD is unclear. In most cases, there is a strong genetic basis. Environmental factors also seem to play an important role in the the development of the condition.
Teenagers and Social Media
Media use has been burgeoning in the last few decades. The majority of adolescents in most developed countries now have 2 or more media/technology devices in their bedrooms. Additionally, most of these adolescents use technology and media for several hours a day. Adolescence is the second developmental phase where rapid, intense neural circuitry development is taking place. The prefrontal cortex of the brain, the part of the brain that has been implicated in inhibition of impulses, organization and attention, undergoes significant developmental changes during this period.
ADHD and Social Media
A recent study, reported in the Journal of the American Medical Association (JAMA), suggests that teenagers who frequently use digital social media may be at greater risk of developing ADHD1. Research has shown that individuals with ADHD are more likely to be high users of video games. This study explored the likelihood of the reverse trend – whether high video game use is linked with increased propensity of ADHD symptoms.
The research team examined adolescents’ ADHD symptoms following use of ‘modern media’, as compared to previous studies on this subject that have looked at ‘traditional media’. Modern media use is characterized by its significantly faster rate/frequency and ‘high intensity’ stimulation’. Modern media is also distinct in terms of offering extensive social connectivity, thereby making it more appealing to adolescents. The team measured adolescents’ ADHD symptoms at baseline and then every 6 months, over a 2-year follow-up period.
The authors reported an association between media use and the development of ADHD symptoms in these adolescents over a 24-month period. Although this finding suggests that media use could potentially be implicated in the development of ADHD symptoms, the association as reported does not prove a causal link.
Frequent notifications, high stimulation, ‘rapid feedback’, immediate accessibility, may all be factors underlying this link, given that these promote the frequent attention paid to media devices rather than to other tasks that adolescents may be engaged in. The authors also describe several, alternate mechanisms by which this association could be explained. Further research is needed to fully understand and establish this association.
ADHD – Recommendations for Lifestyle and Social Media Use
Previous reports have also shown that media devices usage increases the likelihood of shorter sleep duration and poor sleep quality in children and adolescents. We know that inadequate and unrestful sleep can affect attention. This is another area that needs further exploration.
We live in a world where technology and how we use it is changing daily. Social media is a fact of our lives, and it inevitably affects how we pay attention. Some types of media use can have certain benefits for children and adolescents. For developing brains, however, it is important to consider how families might use social media as safely as possible. To this end, the American Academy of Pediatrics (AAP) has released policy statements 2,3,4 that include the following recommendations:
- In children older than 2 years, limit media to 1 hour or less per day of high-quality programming
- Avoid fast-paced programs, apps with lots of distracting content
- No screens 1 hour before bedtime, and remove devices from bedrooms before bed
- For children ages 6 and older, place consistent limits on the time spent using media, and the types of media, and make sure media does not take the place of adequate sleep, physical activity and other behaviors essential to health
- Designate media-free times together, such as dinner or driving, as well as media-free locations at home, such as bedrooms
Additional Resources
References
- Chaelin K, Junhan Cho, Matthew D. Stone, et al. Association of Digital Media Use With Subsequent Symptoms of Attention-Deficit/Hyperactivity Disorder Among Adolescents. JAMA. 2018;320(3):255-263
- AAP COUNCIL ON COMMUNICATIONS AND MEDIA. Media and Young Minds. Pediatrics. 2016;138(5): e20162591 http://pediatrics.aappublications.org/content/138/5/e20162591 Accessed September 13, 2018
- AAP COUNCIL ON COMMUNICATIONS AND MEDIA. Media Use in School-Aged Children and Adolescents. Pediatrics. 2016;138(5): e20162592 http://pediatrics.aappublications.org/content/early/2016/10/19/peds.2016-2592 Accessed September 13, 2018
- Reid Chassiakos Y, Radesky J, Christakis D, et al. AAP COUNCIL ON COMMUNICATIONS AND MEDIA. Children and Adolescents and Digital Media. Pediatrics. 2016;138(5): e20162593 http://pediatrics.aappublications.org/content/138/5/e20162593 Accessed September 13, 2018
5 Ways to Help Children and Young Adults Cope with Depression
Adults who have depression find it difficult to deal with the symptoms of anxiety, insomnia, loss of appetite and guilt while bearing the weight of the world on their shoulders. Children who don’t have the capacity to deal with emotions and who struggle to reach out for support can find it even more difficult to cope with a mental illness such as depression. It is important that children and young adults – as well as their parents – learn how to live with depression. Below are five ways to help children and young adults cope with depression.
1. Be their safety net
As a parent, it’s important to firstly recognize that your child or teenager is suffering from depression. Look for symptoms of declining school performance, such as dropping grades, fatigue, and warning signs such as regular routines that are being disrupted. If you suspect that your child is suffering from depression or has suicidal tendencies, seek help immediately. Consult a professional and find out how you can support your child. Be sure to lock away any medicine, weapons or alcohol at all times.
2. Establish healthy routines
If your child has been diagnosed with depression, it is important to maintain healthy routines that help to ensure enough sleep and encourage physical wellness. A healthy diet can sometimes ease symptoms associated with depression such as fatigue, insomnia and stress. Limiting exposure to technology and harmful social media influences is an important step towards protecting your child’s mental health. Encourage your child to socialize in environments that you know are stable and safe.
3. Spend quality time with your child
Children and teenagers who are feeling depressed tend to withdraw from their environment and seek isolation from family and friends. When this happens, continue to make your support known by being present and by offering support and encouragement. Celebrate small victories with them on their good days and be there for their bad days – even if this means just letting them know that you are present and ready to talk at any time. These tips on how to spend quality time with your kids offer great ideas for showing your support in subtle yet effective ways.
4. Treatment
Cognitive behavioral therapy (CBT) is generally the first line, evidence based psychotherapy for depression; in mild depression, it may be used alone; in moderate to severe depression, it is usually combined with other interventions such as medications. Other therapies that have been shown to be helpful for depression include dialectic behavioral therapy (DBT) and interpersonal psychotherapy (IPT). Antidepressants may be recommended for children or teens suffering from moderate to severe depression that is significantly impairing their functioning.
5. Take care of yourself
Educating yourself about your child or teenager’s condition is important in helping them recover from depression. At the same time, it is also important to take care of your own needs. A healthy parent who takes care of the family and themselves is essential to creating a stable environment. Maintaining a healthy eating routine, getting enough sleep and regular exercise – in which the whole family can be involved, such as taking a long walk or playing some active games together – sets a great example and encourages children and teenagers with depression to get involved. Finding a peer group of parents who are going through similar experiences can be helpful for all the family as they cope with supporting a child or teenager affected by depression.
See our additional resources on depression and mental health.
Remembering What It’s Like To Be Thirteen: Eighth Grade Movie Review
The Challenges of Being a Teenager
It’s easy to forget just how it hard it is to be thirteen. Bo Burnham’s new movie, Eighth Grade, reminds us of these difficulties, with stunningly impressive force. The loneliness, the self absorption and awkward interactions that are all mainstays of the middle school years are rendered with total honesty by Kayla, played by the very talented Elsie Fisher. The events of the film all occur during Kayla’s final week of 8th grade. Kayla is an aspiring YouTube star, who despite the earnest life advice she shares on her channel, finds it nearly impossible to make friends at school. Simultaneously terrified to begin high school and impatient to leave middle school behind, Kayla occupies a kind of awkward, liminal space that people of all ages will recognize.
Growing Up in the Era of Social Media
Kayla has grown up in the age of technology and social media, in a way that informs her, and anyone near her age, experiences. However, it is important to note the nuanced way Burnham approaches the role of technology for Kayla: as both a source of anxiety while still acknowledging the more positive role it can play in adolescent life. In this way, Burnham is able to accurately depict the way technology influences of all our lives, Kayla just happened to grow up using it. Oftentimes, social media is blamed for all of society’s ills, but to do so, the film seems to say, is to negate just how important it can be in people’s, particularly teenagers’ lives.
Teenage Anxiety
The film is also very authentic in its depiction of Kayla’s anxiety. We see Kayla having what appears to be a panic attack in a bathroom, but after she emerges, no one is able to tell; an experience anyone with anxiety will recognize. Kayla’s anxiety is never discussed outright, however, once Kayla is able to recognize how difficult social interactions are for her particularly because of her constant “worrying”–as she describes it–she is able to set some positive life changes in motion. Navigating social situations as a teenager is hard and navigating social situations as a teen with anxiety is even harder. The movie’s treatment of Kayla’s anxiety is a very sympathetic one, which is no doubt accomplished by Burnham’s own experiences with anxiety.
The Reality of Being a Teenager
Despite never relying on common troupes that often ruin movies about teenagers, by the end of the film, Kayla’s life seems to be changing for the better. It is the commitment to depicting an authentic teenage experiences–acne, loneliness, anxiety and all–that make Eighth Grade such an important film. So often, Hollywood makes it nearly impossible for teenagers to see the messy reality of their lives reflected in the glossy sheen of the films that populate the teenage movie canon, magnifying the feelings of inadequacy so central to teenage emotions. Eighth Grade seeks to remedy this.
How to Keep Going When It Feels Impossible
The frustrating thing about anorexia, is that for many the voices will stay in your head for a very long time. At times, they will shout louder, push you around and make you feel like you want to give up. You will start to battle back and put on weight, but as your weight goes up, the mental side of things may take slightly longer to catch up. And at times you will feel like recovery is not possible. Like it is totally impossible and whatever you do won’t help.
I am not telling you this to dishearten you, but to be realistic with how things really are going to be.
I developed anorexia when I was 13 years old and managed to hide it for the next four years. I became a master of deception, hiding everything from everyone around me. I loved having this secret that made me feel so good about life. My anorexia was like having a best friend constantly with me at all times. I relied fully on her, and I loved what she gave me. That value… and purpose…
But all too soon my naughty little secret was discovered and I was no longer able to hide. I was under constant watch from my family and started to go to the Child and Adolescent Mental Health Center. I went there for about six months before being admitted to a mental health hospital where I spent the next year in recovery. I had to learn how to eat, how to exercise in a healthy way, and how to talk about how I felt. It was a tough year, and a battle that I have to keep fighting, but the skills I learnt in hospital had equipped me to do just that.
Recovery from an eating disorder is hard work, but the exciting thing is that when you get to that place in your recovery, life really does start looking up. You can start going out for meals, you aren’t constantly thinking about calories… Life begins to make sense again.
Here are a few things that helped me get to that point, and also continue to help me stay on track when things seem impossible again.
Have People Around You Who Support You and Push You
This isn’t a plain sailing choice and sometimes the people you think are helpful are less helpful as you go through your recovery. What I realized I needed was people I trusted, people who put up with my good and my bad days, people who would hold my hand through difficult meal times, and people who I could ask if I looked “bigger” and they would tell me. But also people who would challenge me in my recovery, help me push those boundaries in a safe place. For me, this has included making a list of 28 things I want to be able to do by the end of the year, such as eating ice cream. I have people round me who push me in this and challenge me to try things. But these people are there afterwards if I find it hard.
Know Your Triggers
This takes time to develop and these might change over time. For me, my main ones are exercise, counting my calories, and big food events (e.g. Christmas). So I know that when I exercise too much I am normally stressed or struggling in other parts of my life. When I relapsed, my exercise did feel out of control again so instead of letting my anorexia win and letting it convince me that I should be exercising more, I got myself a personal trainer. This helped me get my exercise back under control, and now if it flares up I talk about it and tell someone I am struggling with it.
I know that I am likely to find Christmas and other such events quite stressful, but I also know I am strong enough to do them. Over the last few years, I have tried two things with this (and both were successful). First, I cooked the entire Christmas lunch, which meant I felt more in control of when food was coming. And second, planning the meals and day so I know when things were happening. I also always make sure that I go out for a walk on Christmas Day on my own to help process. I am not saying it is always 100% plain sailing, but this helps me feel more okay about it and allows me to enjoy the day.
Remember Your Motivations
My final one is my motivations. Anorexia makes you feel invincible, but the reality is it is everything but that. I had to realize all the things I wanted to do with my life that I wouldn’t be able to do it if I was still living with anorexia dictating my life – things like traveling, getting a job, and having my own family. I urge you to think of your motivations, and at the beginning of meals if it is a struggle, get these out and use them to push you through.
I know how hard it is. I was once someone who thought I would never be able to wear a bikini. I thought I would always have fat days and that I would never be able to stop counting calories. But over time, and with work, I managed to get rid of these thoughts. I realized that beating anorexia was the way forward, and I knew I wanted to keep fighting and I was never going to give up. Yes, there would be hard days, but I would always win! And the more fights I won the easier things would get.
That’s exactly what happened, and I am now in a place where I challenge my eating, push myself in ways that would have previously scared me, and I keep winning my battle against anorexia.
Related Links
Change.org article on eating disorders, weight, and scales
Damon: A Real Life Osteosarcoma Hero
“Strength isn’t how much one can lift. Strength is how much one can lift others!” – Damon Billeck
Meeting Damon For the First Time
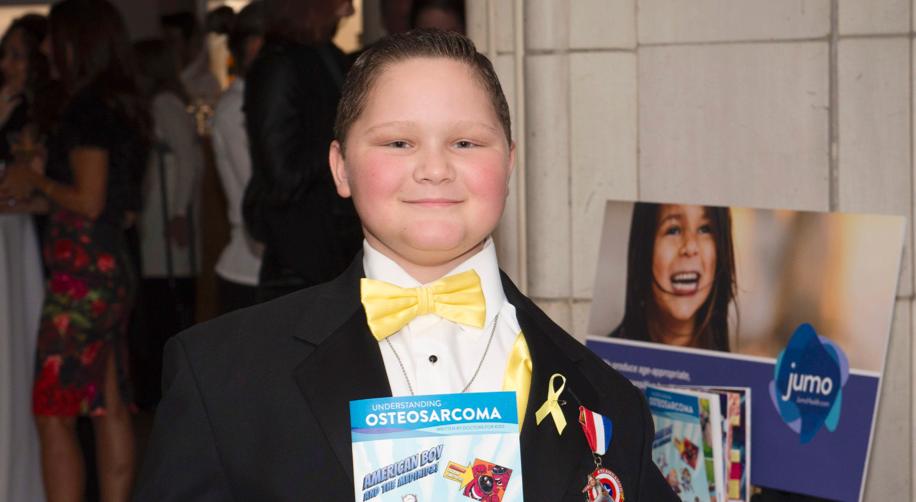
The first time we met Damon, he was on his way to present the Courage Award at the Sarcoma Foundation of America’s Annual Gala, an award that he had received the previous year. Dressed in a tux with a yellow vest and bow tie – the color of sarcoma awareness – we were thrilled to meet the star of our Understanding Osteosarcoma comic book. Everything about him was inspirational, particularly his sunny disposition and eagerness to help others no matter how he was feeling. Whether recording a video with words of encouragement for others battling cancer, or delivering gifts to those in the hospital over the holidays, his desire to help others was evident in everything he did. Sharing his story with the world through our Understanding Osteosarcoma comic, in the hope that it would ease the fears others may have when diagnosed speak to this giant of human being.
The Importance of Spreading Awareness and Sharing Your Story
Having a medical condition can seem isolating. Each day we try to bridge that gap by providing resources that engage and, through the experiences of others, inspire.
The story presents Damon as a superhero (we’ll get to why later) and includes members of his family as well. Both on and off the page, Damon was truly his twin sister Dara’s very own superhero. A lover of Captain America, Damon was diagnosed with osteosarcoma at age nine, and passed away this spring, four years later. Reflecting on Damon’s participation in creating the comic book, his father shared, “that was his crowning achievement, he loved carrying out his story and helping others get through it.”
Damon was a hero to many, including the “real” Captain America, Chris Evans. Damon shared his comic with Evans, because, as his father says, “Damon wanted his hero to see him as a hero.” And Captain America did not disappoint when he autographed Damon’s comic book and continued their support for one another on social media.
July is Sarcoma Awareness Month. We remember Damon as we continue to fulfill his hope that other children and their families might benefit from hearing and understanding his personal and courageous story.
Learn More about Damon’s Story, Osteosarcoma, and the Connection to Captain America Chris Evans
- Read the comic
- Watch Damon’s words of encouragement
- Sarcoma Foundation of America
- See Chris Evans’ tribute to Damon
Childhood Depression
Rates of childhood depression have been rising in the last several years. Yet, information and awareness about childhood depression has not caught on at the same rate. Millions of people across the world wonder and doubt if children can get depressed. Many well-intentioned adults still believe that children can’t get depressed. They are so young- what do they have to be depressed about? When we were that age, we were just happy’. Alongside misunderstanding is stigma and the idea that mental illness is a taboo subject.
What we now know:
- Childhood depression is a real, distinct clinical entity.
- It is a serious health condition, which if left untreated, increases risk of future, prolonged and more severe depressive episodes. Untreated depression in childhood and adolescence can pose risk of suicide.
- Depression often has biological, psychological and social underpinnings. An individualized treatment plan that explores and addresses each of these aspects, works best.
- Effective treatment options for childhood and teen depression have been widely tested, proven and established, through several scientific studies over the years.
- Childhood depression can be hidden and therefore, easily missed. Timely recognition and treatment can be life-changing and life-saving.
- The barriers surrounding mental health stigma are beginning to give way due to powerful social movements and discussions that address realities of mental health.
Who is Affected by Depression in Childhood or Teenage?
Depression can affect anyone. However, children or teens who have immediate family members with a history of depression or other mood disorders (such as bipolar disorder) are more likely to suffer from depression, often due to a genetic predisposition.
Predisposition implies greater likelihood; it does not mean that the child or teen will necessarily experience depression.
Children with chronic or severe medical conditions are at a greater risk of suffering from depression.
Common Signs of Depression in Childhood or Adolescence
Depression in childhood/adolescence can manifest somewhat differently than it does in adults. Irritability and/or anger are more common signs of depression in children and teens.
When depressed, younger children are more likely to have physical or bodily symptoms, such as aches or pains, restlessness, distress during separation from parents, as they may not have the emotional attunement and/or expressive abilities to talk about their emotions.
Other signs of depression in children and teens, can be:
- Loss of interest in usual fun activities
- Withdrawal from social or usual pleasurable activities
- Difficulties with concentration
- Running away from home or talking about running away from home
- Talking about death or dying, giving away (or talking about giving away) favorite possessions, writing goodbye letters
- Sleep increase (or decrease)
- Appetite/weight changes (more likely an increase, in depressed teens)
- Occasionally, new or recent onset agitation or aggression
- Comments indicating hopelessness or low self-worth
Not all of the above-mentioned symptoms have to be present for a diagnosis of depression. Symptoms usually occur on most days, for at least 2 weeks, in order to meet criteria for depression. When seeing a professional to explore a diagnosis, you can utilize online health resources to prepare meaningful questions to ask a doctor in order to facilitate productive conversation for treatment.
Ruling Out Medical Conditions First
Psychiatric disorders are diagnosis of exclusion, which means that only if the symptoms are unexplained by medical conditions, or effect of substances or other non-psychiatric causes, would the cause of symptoms be deemed to be due to a primary psychiatric disorder.
Before arriving to the diagnosis of depression, a child or teen who is suspected to be depressed, must undergo a comprehensive medical evaluation to rule out any underlying medical condition which could be manifesting as or resulting in depression. For example, hypothyroidism (depressive symptoms, weight gain, low energy, cognitive difficulties, constipation). Even conditions such as undiagnosed anemia can mimic depression, due to accompanying fatigue/low energy. Vitamin D deficiency, common in cold climates, increases risk of depressive symptoms and fatigue. The good news is that these conditions have effective treatments, and treatment of the underlying medical condition in a timely manner should resolve depressive symptoms.
Ruling Out Other Psychiatric Conditions
Rule out undiagnosed/untreated ADHD (attention Deficit Hyperactivity Disorder), anxiety disorders or other psychiatric conditions, which when left untreated, can result in depressive symptoms due to the impairment in functioning from ADHD or anxiety disorder itself.
Treatment
Why Treat?
Depression is associated with visible brain changes seen on functional brain MRI studies of depressed individuals. Treatment, for example, psychotherapy has been shown to confer long term benefit and neural changes in the brain.
How Do I know My Child Needs Treatment?
In addition to an overall assessment, your child’s pediatrician may administer rating scales and other forms of assessment to determine the degree of depression and may refer you to a psychiatrist or a psychotherapist.
We know a child/teen needs treatment for depression when their school, social, and/or home functioning is significantly affected by depressive symptoms, on a frequent basis.
If your child/teen is feeling suicidal and/or having thoughts/urges to hurt themselves, call 911 or take your child/teen to the nearest ER.
What Kind of Treatment?
For mild to moderate depression, CBT (Cognitive Behavioral Therapy) is the typical first-line treatment of choice for children and teens. There can be exceptions to this, depending on the specific clinical condition, age and circumstance of the child. For children younger than 10, other modalities of psychotherapy such as play therapy, psychodynamic psychotherapy, and behavior therapy may be utilized.
For moderate to severe depression, evidence-based guidelines recommend a combination of CBT and antidepressant medications (typically SSRI medications, also known as Selective Serotonin Re-Uptake Inhibitors).
SSRI Use for Depression in Children
- SSRIs and other antidepressants have a black box warning from FDA about risk of increase in suicidal thoughts and behavior with use, particularly in the early phase of treatment. Studies did not show completed suicides.
- After this warning came out in 2004, antidepressant prescription rates dropped, and suicide rates climbed up.
- Close monitoring during dose initiation, titration and dose changes helps to reduce this risk
- Antidepressant medication use in children and adolescents is preceded by a weighing of benefits and risks of use versus risks of untreated depression.
- Fluoxetine and Escitalopram are FDA approved for treatment of depression in children and teens.
- Studies involving paroxetine (another SSRI) have shown a higher profile of side effects with its use in children, and therefore, may not be recommended for children and teens.
- Studies show a higher likelihood of an individual responding to an SSRI that an immediate family member benefitted from (however, this is a likelihood, not necessary that it will happen in each situation)
If depressive symptoms are secondary to other conditions, such as untreated ADHD or anxiety disorders, adequate treatment of those disorders is essential and will usually resolve the depressive symptoms. However, in certain situations, specific antidepressant medications and/or psychotherapy targeted towards depression may be needed in addition. One might note that if trials of two or more antidepressants are not effective, or if a child/teen is sensitive to medications in general, there are additional avenues that can be explored. One plausible route for consideration is genetic testing that combines personal genetic data with medication information to achieve the desired remedy.
Your child’s pediatrician/psychiatrist, therapist, together with you, may also explore for any bullying, trauma, and will try to understand your child/teen’s inner life and look further for any school, social, family or other stressors that may be contributing to, or exacerbating/perpetuating the depressive condition. If family stressors are significantly contributing to your child’s depression, your doctor may recommend family therapy in addition. With your permission, the doctor/therapist may coordinate with your child’s school to share recommendations to optimize your child’s school functioning and emotional well-being at school.
Overcoming Mental Health Stigma
In 1999 the United States Surgeon General labeled stigma as quite possibly the biggest barrier to mental health care. Stigma manifests as misguided stereotypes and negative attitudes or beliefs towards those with mental illness. Research shows that stigma and embarrassment were the top reasons why people with mental illness did not engage in medication adherence, such as self-care, therapy and medication compliance. As of late, there has been an increase in available resources and tools to overcome stigma for children and teens, as well as their caregivers. Allies such as Bring Change to Mind, an organization focused on encouraging dialogue about mental health, as well as raising awareness through education, offers high-school and college programs that foster a culture of peer support within schools.
A Word About Substance Use and Depression
Sadly, substance use among teens is becoming rampant across the country, even in reputed school districts, and thus, needs to be addressed when exploring and treating depression.
Marijuana use is particularly common among teens. Marijuana is considered to be a ‘gateway drug’ and can lead to ‘amotivational syndrome’. This syndrome manifests as low motivation to do things, and in conjunction with marijuana related ‘munchies’ can mimic a primary depressive disorder. In many cases, a teen may be ‘self-medicating’ for untreated or undiagnosed depressive or anxiety symptoms through substance use. Use or withdrawal from other substances can cause depressive, mood symptoms as well.
Proper and timely treatment can be very effective in resolving depressive symptoms and in reducing risk of relapse. Please consult your child’s pediatrician or health care provider if you suspect your child/teen may be suffering from a medical or a psychiatric condition.
Note: This article is for informational purposes only and is not intended to provide medical or psychiatric advice or recommendations, or diagnostic or treatment opinion. This is not a complete review or description of this subject. If you suspect a medical or psychiatric condition, please consult a health care provider. All decisions regarding an individual’s care must be made in consultation with your healthcare provider, considering the individuals’ unique condition. If you or someone you know is struggling, please contact the 24×7, confidential National Hotline at 1-800-273-8255 or use the crisis text line by texting HOME to 741741 in the US, or go to http://www.suicide.org/international-suicide-hotlines.html for the suicide hotline number for your country.
Type 1 Diabetes Research Spotlight | Bringing New Life to an Old Vaccine
Diabetes Researchers Leave No Stone Unturned
My whole life I had taken my pancreas for granted. That is until my now 2-year old daughter was diagnosed with type 1 diabetes (T1D) at 13 months, and myself, 3 months ago. I’ve since become fixated on and fascinated by the research advancements being made in attempt to mimic the meticulous 24/7 work of the pancreas. The most recent discovery demonstrates how one of the world’s oldest vaccines may have potential to regulate blood sugar.
Type 1 diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. Because the pancreas is no longer able to make insulin, type 1 diabetics must take replacement insulin—via an injection or insulin pump—every day and with every meal. The Bacillus Calmette-Guerin (BCG) vaccine, or TB vaccine has been used against tuberculosis for nearly 100 years. The connection between the two? Researchers at Massachusetts General Hospital found that adults with established T1D (at least 10 years) treated with the TB vaccine had blood sugar ranges return to near normal levels.
Eight-year follow-up results from a Phase I clinical trial were published yesterday in the journal NPJ Vaccine. After receiving 2 doses of the TB vaccine, about 50 people with T1D saw a delayed, yet significant drop in their long-term average blood sugar levels, which was sustained over the next five years of the study. And no cases of severe hypoglycemia (low blood sugar) were reported. Patients also saw their average A1C drop from 7.4% to 6.2%. A1C is an average measurement of blood sugar levels over a two-to three-month timeframe. The American Diabetes Association recommends an A1C of 7% or lower for diabetics. Lowering blood sugar and A1C reduces the risk of complications associated with diabetes, such as eye, kidney, and nerve damage.
How can a TB vaccine lower blood sugar? By eating sugar!
“[TB] changes the metabolism, and it eats sugar for its energy source,” Dr. Faustman, director of Mass General’s immunobiology laboratory, explained. When BCG is administered to people with Type 1 diabetes, defensive white blood cells called lymphocytes gain an increased taste for sugar too; they switch their normal energy consumption habits to a process called aerobic glycolysis, which allows them to “eat more sugar for energy.” BCG may even play a role in “re-training” the immune system to stop attacking insulin-producing cells.
Is this a cure? Not quite yet. Patients still needed to take insulin. However, less may be needed, and blood sugars may be more controlled. Research is still in its early stages to draw any finite conclusions, but it offers hope for easier management of this unpredictable, relentless disease.
My dream is for a cure during my daughter’s lifetime, so that she can experience life without the constant anxiety over blood glucose numbers.
Take time today to thank your pancreas!
Not all content is created equal
We produce content differently at Jumo Health, check out our Understanding Type 1 Diabetes digital comic and take a listen to our podcast roundtable discussion on T1D and U. Browse all of our age appropriate diabetes resources and curated content. #OwnYourHealth
Our Mental Health Awareness Pledge
A Pledge For Mental Health Awareness
May has come to a close, and so have a number of Mental Health Awareness campaigns. Devised in the U.S. in 1949 by the Mental Health America organization, Mental Health Awareness Month is dedicated to raising awareness and educating the public about mental illness, some form of which affects approximately 45 million adults and 17 million children.
Today, more organizations and institutions than ever before are choosing to take part in a mental health awareness campaign each May, including Jumo Health. This past month, we dedicated ourselves to getting our community involved to #StopTheStigma that prevents more than half of all those who suffer from anxiety, depression, and other forms of mental illness from seeking the help they need.
Continuing a Critical Conversation
However, one month is not enough. Creating the kind of healthy cultural conversation that will end the harmful stigma means continuing to talk about mental health beyond May and weaving the topic into our societal fabric and our daily lives.
Physical and mental health are two sides of the same coin, and we must carry on the kind of progressive dialogue that’s so prevalent in May if we want to do away with the guilt, shame, and isolation that so many individuals confront when dealing with mental illness.
This is why we at Jumo Health have decided to invoke the following Mental Health Pledge:
We pledge, as an organization, to ensure the inclusion, where appropriate, of mental health considerations in all of our resources as we strive to stop the stigma commonly associated with mental health conditions.
The conversation around mental health needs to change – and that begins with awareness and education. Mental illness presents itself in different ways, at different times, and does not discriminate. For us at Jumo Health, that means naturally integrating mental health topics into our content and tools.
Make Your Pledge
Join us in making mental health awareness a lifetime campaign. Find and connect with us on Facebook, Twitter, or Instagram, where we’d love to hear your story or how you’re pledging to #StopTheStigma and #OwnYourMentalHealth. Tag us @jumohealth and we can continue the conversation together.
Silent No More
My friend died by suicide.
Hearing that someone has taken his or her life invokes feelings of anger, sadness and, regretfully, judgement.
On March 7, 2008, my dear friend said he had a surprise gift for me. “Too” busy, I didn’t have time to meet. Months later, he was gone.
In the days and months following his death, I found myself wondering – if I had been more available, more present, could I have recognized the warning signs?
My friend had bipolar disorder. It was the first time I was directly affected by mental illness.
While some of my friends know about the suicide, I have never shared the “part of the story” that has to do with me and my guilt – until now. I’ve been too embarrassed, wondering what I could have done to help prevent it. So I remained silent.
Although I eulogized him at his memorial service, I can count the number of times I’ve talked about his suicide on one hand. I am still emotional over the experience. But, in honor of mental health awareness month, and our pledge at Jumo Health, my silence ends today. By talking about my experiences and using our voice at Jumo Health to create patient and family centric products, we hope to help bolster the conversation surrounding mental illness.
Let’s Act
At Jumo Health, we often hear about the feeling of empowerment derived from peer to peer learning. Sharing is, indeed, cathartic. For us at Jumo Health, that means ensuring there are credible, age appropriate and culturally sensitive resources available on a global scale. We hope this can encourage greater openness and a dialogue around health care – at home, in the media, and in the classroom. Breaking the silence means understanding the role mental health plays throughout health care and in our daily “normal” lives – directly and indirectly.
Let’s Share
As Jumo Health’s Rebecca Schelkun shares in our In My Words podcast series, “50% of all cases of mental illness begin by the age of 14. Even more alarming is that suicide is the second leading cause of death for those aged 15 – 24.” In conjunction with Mental Health Awareness Month, we’re releasing podcasts episodes of conversations with patients and physicians.
Our podcast series takes individual stories, often kept stored away, and brings them to light. We share these stories so that those in need can learn from the experiences of others, to gain the strength to persevere by listening to messages of hope, to encourage those affected to step out of the darkness, seek support or care, and break their silence.
Those interested in listening can stream or download the In My Words Podcast.
I’ve been in health care my entire career – addressing the needs of both providers and consumers. Intellectually, I understand what happened to my friend was the result of a disease. I understand that I had nothing to do with his suicide. It is this disconnect, this misunderstanding of mental illness that perpetuates the stigma surrounding it and what hinders the conversation.
After 10 years, I still think of my friend often. He left his mark and I remain thankful for knowing him and sad that he’s no longer with us. I look forward to honoring Jumo Health’s pledge and his legacy by participating in the conversation.
Collectively we can #StopTheStigma