Managing Your Child’s Diabetes: Preventing Burnout
Courtney Taylor is a mom (Chase, 10 & Carter, 6), educator, and advocate living in Philadelphia, PA. Chase was diagnosed with Type 1 Diabetes when he was three years old. Courtney and Chase are the founders of The CHASE away Diabetes Foundation, 501(c)3—a non-profit organization committed to raising awareness and influencing advocacy for Type 1 Diabetes.
Courtney reflects on her experience over the past 7 years, and offers advice for those in a similar situation.
If I Knew Then What I Know Now: A Letter to My Younger Self
August 20, 2011
Dear Courtney,
Before you read this letter, grab a box of tissues, pour a glass of wine (it’s okay to fill it to the brim), and find a quiet space where you won’t be interrupted. Trust me. Today is the last day you will feel the way you do; tomorrow, everything will change. The changes you’ve been noticing in Chase—bedwetting, mood swings, and extreme thirst—are all about to make sense. Chase (take a deep breath) has diabetes. Breathe. The doctors will diagnose him tomorrow and you will spend days in the hospital learning how to live as a family with this illness. It won’t be easy, and no matter how many people say it will—it won’t get easier. So, here’s what I want you to do. Cry. Cry as long as you want, as loudly as you want. Be angry—but don’t stay there. This illness, while manageable, will cost you a lot—mentally, emotionally, physically, and financially. It will require you to be open to constant learning and to educate others. You will also make mistakes, but you must be willing to forgive yourself and move forward. Most importantly, while it’s going to hurt you the most, you are not the one living with it, Chase is, so don’t forget to include him in everything. Lastly, there are going to be days when you just want to throw in the towel and give up—but diabetes doesn’t allow for sick days so here are some things to remember on the worst of the worst days.
Ask for and Accept Help
This will be the hardest to do, so that’s why I’ve included it first. If you attempt to fight this fight alone, you will lose quickly—take advantage of those around you. There’s a village of people who want to learn how to check blood sugars, administer insulin, and count carbs—they’re just waiting for you to teach them. It won’t be an overnight lesson, it will take time. The more people you involve in your child’s care, the more phone numbers you can dial when you need a break.
Forgive Yourself
You are going to put numbing cream on so you can do a site change, and you’ll fall asleep. You are going to need to pick up a prescription in the morning to drop off at school before you go to work—and there will be traffic, so now you’re late for work. You will forget to pack lunch carbs in the lunch bag (more than once). You won’t hear the CGM alarm the first time it goes off. So many imperfect scenarios of how you will “fail” as a diabetes parent, but they won’t be outweighed by all the sacrifices you are going to make—give yourself a break. It’s okay.
Make a Plan
As I stated earlier, this is going to cost you. I neglected to mention the time it will cost. Plan ahead. Your best bet will be to make a weekly menu. Count the carbs ahead of time, and pack lunches and snacks for the week. This will help you feel less anxious in the mornings—especially while you wait for your child to take 40 minutes to put on 2 socks. Also, get a monthly calendar and plan out site changes. They will sneak up on you.
Talk About It
One way to work through feeling burned out is to talk about why you are feeling burned out—don’t forget to cry if you need to. Find a group of parents who know what you are experiencing and swap diabetes stories, talk with family members and share how they can help relieve some of the stressors of being the main caregiver. And talk with Chase—he is walking this journey with you and while it’ll help you cope, it will also give him the language to work through his feelings and thoughts as well.
Include Your Child
In addition to talking with Chase about how you are coping, include him in other conversations. He should be apart of the medical conversations, he needs to know how you are managing his illness, but he also needs to begin to learn how to advocate for himself and that starts with finding the power in his voice. This isn’t limited to doctor visits, he should also be included in the everyday management—from day one; yes, I know he’s only 3. The more involved he is, the stronger he will feel about standing up for himself and educating others.
Tomorrow is a new day, it won’t be easy, but you will make it through.
Love,
Your wiser self
The Promising Future of Type 1 Diabetes Management
Type 1 diabetes (T1D) is an autoimmune disease in which the immune system mistakenly destroys the insulin-producing cells (beta cells) in the pancreas. Insulin is an essential hormone that regulates the amount of glucose in the blood. Because people with T1D can no longer produce insulin, they must continuously monitor their blood glucose and take insulin with every meal to survive.
The “Dark Ages” of Diabetes Treatment
As if managing Type 1 diabetes isn’t challenging enough with constant glucose checks, carb counting, and insulin dosing, imagine if you were living with T1D 75 years ago, prior to the availability of the medical advancements we have today. You would sterilize your needles and large glass syringes by boiling them daily. Sharpen your needles manually using an abrasive stone. Test your urine for excess sugar by heating it in a test tube mixed with a chemical solution. And your blood glucose would only be checked in a doctor’s office once a month! The complications you would inevitably develop from diabetes would be viewed as “normal” and nothing could be done to slow their progression. This is during a time in which the medical community thought it was nearly impossible to regulate a diabetic’s blood sugar. I guess if I was only checking my blood glucose once a month, I’d believe this, too.
Advancements in T1D Care
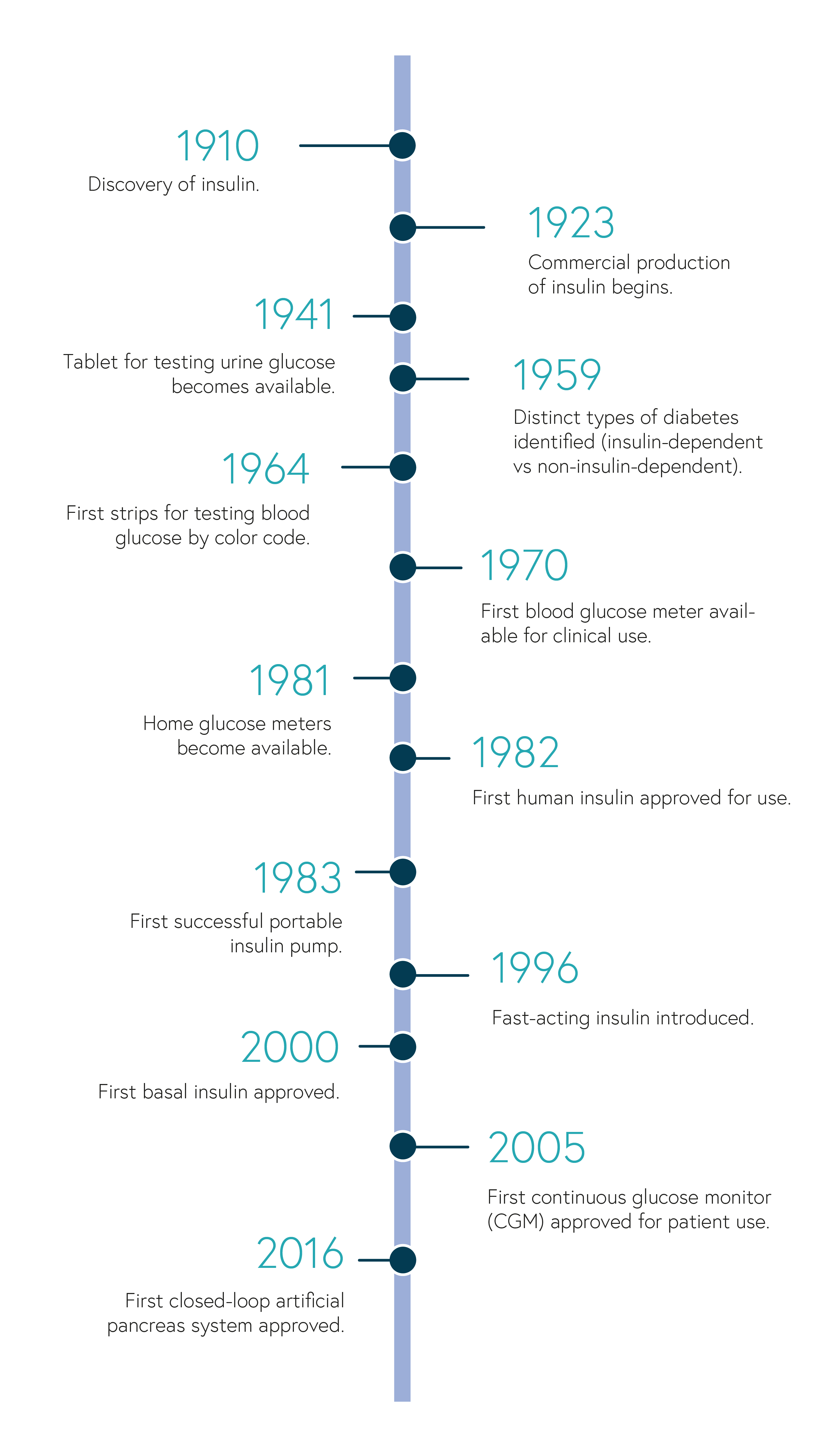
Treatments and technological tools for managing T1D have come a long way in the last 100+ years since the discovery of insulin. This timeline highlights a few of these milestones.
(based on the American Diabetes Association 75th anniversary timeline)
Today, we have disposable syringes, insulin pens, continuous glucose monitors, insulin pumps, and glucose meters, to name a few, and some of which we may take for granted. These tools help people to better regulate their blood glucose and optimize insulin dosing, improving overall quality of life and decreasing the risk for complications. Although scientists still don’t fully understand what triggers the immune system to destroy the insulin-producing beta cells, research is developing rapidly with the goal of achieving blood glucose control while lessening the burden of diabetes management. The artificial pancreas, pancreatic islet transplantation, beta cell regeneration, and smart insulin are only a few of the many exciting advancements that may revolutionize T1D treatment.
- Artificial pancreas (closed-loop system). In 2016, the FDA approved the first closed-loop insulin delivery system, a new technology that connects a CGM with an insulin pump to automatically monitor glucose levels and adjust insulin delivery. A computer-based algorithm receives glucose readings from the CGM, determines the dose of insulin needed, and sends instructions to the pump to release that amount of insulin. The goal of this system is to mimic the function of a healthy pancreas by regulating blood glucose and reducing the occurrence of hypoglycemia (extremely low blood sugar).
- Pancreatic islet (beta cell) transplantation. Islets are clusters of cells in the pancreas that contain insulin-producing beta cells. Healthy beta cells from the pancreas of a deceased donor are injected into a particular vein of the patient with the goal of reducing, or even eliminating, the need for insulin injections. This procedure is limited to certain patients due to the shortage of donor cells and risks associated with transplants. Each procedure injects 400,000 islets, and more than one injection is needed to eliminate the need for insulin injections. As with most transplants, the patient would also need to take drugs to suppress the immune system so that it doesn’t destroy the donor cells. Immune suppression is associated with an increased risk for infection and cancer. Physicians would have to weigh the benefits with the risks when deciding if a patient is eligible for this procedure.
- Beta cell regeneration. Regenerating, or restoring, beta cells in the pancreas would eliminate the need for donor cells. This procedure uses a naturally-occurring growth factor to stimulate progenitor cells—a special kind of cell that can turn into different kinds of cells—in the pancreas to produce more beta cells. Because the immune system in people with T1D attack beta cells, researchers are looking for ways to avoid immune destruction of these newly formed insulin-producing cells without the use of immunosuppressive drugs.
- Smart insulin. Smart insulin, or glucose-responsive insulin is designed to automatically activate or deactivate in response to the levels of glucose in the blood. It would circulate throughout the body, and only activate when blood glucose levels are high. After the amount of blood glucose is lowered, the insulin would deactivate. The smart insulin patch is thin, silicon patch with more than 100 microneedles containing glucose-responsive insulin. Research is still in the early stages, but it is the hope that smart insulin will promote tighter glucose control and lower the risk for hypoglycemia.
With all the promising research taking place, management of T1D can only continue to improve. Perhaps not too long from now, diabetes-related complications and reduced life expectancy will become a worry of the past. For now, I look forward to the day when my daughter and I can indulge in a brownie-bottom sundae without agonizing over carb count and high blood glucose numbers.
Who Are The Diabetics on The Margin?
Creating Your Diatribe
I initially connected with Ariel Lawrence after we had both been interviewed on the Diabetics Doing Things Podcast. At the time, she told me about her partnership event, “Diabetics on the Margin” with Beyond Type 1, celebrating and supporting people of color. I immediately bought a ticket.
When the elevator opened to the Homepolish offices where the event took place, I saw type 1 diabetics of color everywhere. I also noticed a spread of perfectly portioned low-carb breakfast items,emergency gummies, and juices. It was the first time I had ever seen anything like it, and it was magical. I knelt down to check my blood sugar in the corner of the room and was promptly invited to sit in a comfy chair instead (also something that had never happened to me before). I had gotten used to having to take care of myself on the margins at social gatherings. At the Diabetics on the Margin event, being invited to sit at the table (and check my sugar at it) was so empowering that all my shyness immediately disappeared.
Just when I started mingling, I saw two familiar faces – Danielle and Joe! We had gone to high school together, but had lost touch over the years. As I soon discovered, they also have type 1 diabetes. The accidental high school reunion made us newfound “diabuddies” for life. Everyone I met commented on how happy they were to finally find an event like this, after many years of googling in vain for something similar, or joining online groups that did not actually offer a real community or safe space to talk about race and ethnicity in relation to diabetes.
Post initial mingling and snacking (thanks @Sweetsciencechef), the audience took their seats to hear various perspectives from Ariel Lawrence, Ali Abdulkareem, Dr. Maria E Peña, Vivian Nabeta, Courtney Taylor and Chase Dupont, Sarah Lucas and Grace Bonney. Sarah Lucas talked about Beyond Type 1’s mission to provide all the resources people need to connect with one another and manage a life-long condition, as well as their partnership with Ariel Lawrence and other sponsors that made this event possible. Ariel shared with us her reasons for starting the Diabetics on the Margin platform—primarily to support one another. Discussion followed about what real support systems might look like, how best to cope with physical and mental diabetic burnout, and what the people who love us can do to help.
Ariel Lawrence:
“Do your own research, too. Don’t put all the burden on us to educate you.”
Finding the Right Doctor
Endocrinologist Dr. Peña discussed her personal frustrations as a doctor looking after those with diabetes:
“Doctors will overbook, expecting some patients not to show up, because they have pressure from insurance companies to meet patient quotas.”
Courtney Taylor, the mother of 10 year old Chase Dupont (diagnosed at age 3), shared the challenges she had encountered in the health care system from the patient/carer perspective:
“When Chase’s blood sugars were all over the place over the summer, I thought about rescheduling his tri-monthly appointment so I could get him back on track, because I didn’t want to hear from his doctor that I don’t know what I’m doing or that I’m not doing enough for my child…when I’m doing everything I can to keep him alive.”
Following a discussion, it was generally accepted that compromise is needed on both sides—doctors have to be able to discuss management options without being accusatory, and patients have to make an effort to show up or ask if their doctors can provide phone or other guidance about their blood work when they cannot make an appointment. Vivian Nabeta mentioned other socioeconomic reasons for patients not showing up (in America and Africa): distance from the clinic and lack of transportation; having to choose between eating today or paying for a doctor’s visit; and not having access to childcare.
Opposition To This Event and Events Like This
The panelists and audience members had all experienced opposition from those who claimed that such events might be seen as either anti-white, or believed that they should not be separated from more general discussions on diabetes. CEO and Co-Founder Sarah Lucas responded:
“Beyond Type 1 isn’t afraid to say anything and stand behind those whose stories deserve to be told.”
Grace Bonney agreed:
“We have plenty of space. We don’t need anymore space. There’s tons of visibility for white people with Type 1. It is absolutely our job to talk to the other white people who are doing a poor job, to give people of color the space they need to speak on issues that matter to them.”
Similarly, from Ariel Lawrence:
“We’re not excluding white people. We need you to be here as allies so we’re not just preaching to the choir.” When asked what seeing yourself represented here today means to you, Courtney clarified the question for Chase. She asked the audience to raise their hands if they were living with type 1 diabetes and a sea of hands immediately went up. Courtney then asked her son:
“Chase, imagine this is your classroom and you see all these people have type one, how does that make you feel?”
He responded:
“It makes me feel excited…to know all these people know what it’s like to live with this.”
For me, representation is everything. We all need to be able to see ourselves in order to build a real diabuddy support system, to resolve the socio-economic barriers, and to ultimately find our sugar freedom. We can only achieve that when everyone is at the table.
Additional Resources
Diabetes Awareness Month 2018
The Reality of Diabetes
When you hear the word “diabetes” what words first come to mind? “Eat right, lose weight, eat less sugar, preventable, curable”—words often spoken on TV ads or printed on magazine covers. “Constant vigilance, glucose monitoring, anxiety, sleepless nights, carb counting, insulin shots”—these are words that come to mind for someone living with diabetes. Being a type 1 diabetic myself, as well as a mom of a 2-year-old type 1 diabetic, these words are my #EverydayReality.
Diabetes is a common and serious disease. About 30 million Americans currently live with diabetes. And about 1.25 million of these children and adults have Type 1 diabetes. People with diabetes are at an increased risk of serious health complications, including vision loss, heart disease, stroke, kidney failure, amputation of toes, feet or legs, and premature death.
What is Diabetes?
Diabetes affects how your body uses a type of sugar called glucose. Glucose comes from carbohydrates, or carbs, in the foods you eat. Some foods have more carbs than others. A common misconception is that diabetics only need to avoid sugary foods like cakes, cookies, and candy. But most foods, including fruits and vegetables, contain carbs. When you eat, glucose travels through your blood to your cells, which use it for energy. But glucose can’t enter the cells by itself. It needs insulin, a hormone made by your pancreas, to enter the cells. In people with diabetes, glucose has trouble getting into the cells, so it builds up in the blood, especially after you eat.
- Type 1 diabetes is an autoimmune disease. The immune system, which normally protects you from germs, mistakes cells in the pancreas for bad guys, and destroys them. The pancreas can no longer make insulin. All people with Type 1 diabetes must take insulin every day and with every meal, which requires constant monitoring of blood glucose and carb intake. Anyone, at any age, can be diagnosed with Type 1, and it is neither preventable nor curable.
- In Type 2 diabetes, the pancreas still produces insulin, but either the cells start ignoring insulin’s command to let glucose in or, in some cases, the pancreas can’t keep up with the amount of insulin the body needs. Type 2 diabetes can run in the family. People who aren’t a healthy weight, aren’t physically active, or who don’t eat a healthy diet are also more likely to develop Type 2 diabetes. Although medication is sometimes needed, being physically active and staying a healthy body weight by eating right can help manage Type 2 diabetes.
Are There Any Warning Signs?
Common symptoms of diabetes include extreme thirst, hunger (despite eating), urinating often, extreme fatigue, blurry vision, cuts that heal slowly, unintentional weight loss despite eating more (Type 1), and tingling, pain, or numbness in hands or feet (Type 2). Some people with Type 2 diabetes have symptoms that are so mild that they go unnoticed. Many adults with Type 1 diabetes are often initially misdiagnosed with Type 2 diabetes because of the lack of understanding that Type 1 can happen at any age. Children who have symptoms of Type 1 diabetes are often mistaken to have the stomach flu or a virus. About 42% of people with Type 1 diabetes are in diabetic ketoacidosis (DKA) at the time of diagnosis. That means 4 in every 10 people had their signs and symptoms of Type 1 diabetes misunderstood or ignored. DKA is a life-threatening consequence of diabetes, in which the body breaks down fats for energy, releasing acids into the blood called ketones.
The impact of diabetes. Diabetes affects everyone differently, and everyone has their own way of managing and coping with a chronic illness. But just because you can’t see someone’s diabetes, that doesn’t mean it doesn’t affect them every minute of every day. “For the diagnosed, diabetes can affect every decision – what to eat, wear, do, and other decisions about how they’ll take care of themselves. Yet the 24/7 burden of diabetes management is often misunderstood.” –American Diabetes Association
For National Dyslexia Month, Break Out Some Comic Books
Crime fiction writer Jay Stringer is a prolific and celebrated author. But when he was a boy growing up in Scotland, he deeply struggled to learn how to read even the simplest texts. What he discovered later was that he was dyslexic – and more importantly, that he could unlock the literary world through comic books despite his diagnosis.
“I’m dyslexic,” he wrote in an article for Book Riot. “I could have been one of those left behind, but comic books pulled me out.”
Stringer is far from alone. Over the years, those with dyslexia have discovered time and time again that comic books and graphic novels are wonderful — and sometimes vital — resources, both for initially learning to read and for truly enjoying reading.
Why? These books pair illustrations with words, allowing readers to glean information from more sources than words alone. At the same time, they don’t contain huge blocks of text, which can be overwhelming, intimidating, and tiring for those who struggle to process the written word.
“Comics were a clever trick to entice me into reading more even after I was tired of working that part of my brain,” said James Barclay, another person with dyslexia who found comic books were vital in helping him learn to read, stay interested in reading, and follow written narratives.
Today, comic books and graphic novels are firmly established learning tools for students with a dyslexia diagnosis — not to mention enjoyable reads for any student who loves mixed media and page-turning action.
During Dyslexia Awareness Month, consider donating a few graphic novels or comics to your local school or library, checking out some books yourself, or simply learning more about what dyslexia is as well as what it isn’t.
Making Comic Books Even Better For Readers With Dyslexia
While comic books are great for readers with dyslexia, there are a few simple changes that comic book publishers could make to increase accessibility even more. Writer Christine Ro points out that comic book fonts could be improved so that are easier to read. Currently, traditional comic book style involves all-caps dialogue, when those with dyslexia find it easiest to read mix-capped, sans-serif fonts.
Learn more about dyslexic-friendly fonts and styles here.
It’s Also Health Literacy Month
In addition to Dyslexia Awareness Month, it’s also Health Literacy Month, a month that is all about focusing on reading, understanding, and acting upon health information. Did you know that 9 out of 10 adults have difficulty utilizing health information that they read — and that there are often not readily-available age-appropriate resources for kids who are diagnosed with health issues or conditions?
This month, and every month, make an effort to learn more about health literacy, whether you are better trying to understand a dyslexia diagnosis for you or your child, or trying to learn more about any disease, illness, or condition.
Here are some quick tips:
- If you don’t understand something, ask your doctor to use more familiar language.
- Take notes during doctors’ appointments or while reading health literature. Write down questions to ask your doctor or health provider.
- Ask your doctor to direct you toward appropriate, accurate resources after your appointment.
- Ask your local librarian for help seeking accurate health information, either in books and article or from online sources.
- Check out Jumo’s age-appropriate health resources for the whole family.
The Connection Between Screen Time And Teen Mental Health
There has been a shocking 33 percent surge in depressive symptoms among teens, beginning around 2012. While a number of factors may contribute to this trend, there is mounting evidence that one of the main causes is screen time, online browsing, and lack of face-to-face interaction.
Specifically, studies have found that Facebook causes declines in youth happiness, that new media screen time increases depression and suicide-related outcomes in teens, and that teens are replacing sleep with time online, and suffering mental health consequences.
The harm of screens comes from a variety of sources. First and foremost, time spent on screens is time spent isolated from others, when face-to-face interaction is a mainstay of mental health. Secondly, time spent on social media sites is found to harm life satisfaction, across basically all demographics. Finally, screen time hurts the time and quality of sleep, when sleep is intimately connected with mental health and depression in young people.
What can parents do to best limit their kids’ screen time and help protect them against depressive symptoms? While it can often feel like you’re fighting a losing battle against the onslaught of technology, there are a number of simple steps you can take to turn off the screens and encourage other healthier activities both in and out of your home.
Tips For Limiting Teen Screen Time
While we can’t say for certain that screen time can cause depression in teens, there is enough evidence that the two are strongly correlated that most experts agree that limiting screen time is beneficial to children. Here are a few of the best ways to limit screen time in your household.
- Set limits. Teens spend an average of nine hours a day consuming media – and not all media is created equal. Experts suggest the upper limit for kids under 18 should be 2 hours of recreational screen time per day. In addition, the more of that time that is dedicated to enriching and educational screen time, the better.
- Encourage face-to-face interactions. One of the reasons researchers think screen time is harmful is because it takes away opportunities for real human interaction, which is proven to boost mental health. At the same time you discourage screen use, you should encourage social activities like playing with neighborhood kids, participating in after school sports, and eating meals as a family.
- Ban screens from bedrooms. Many kids are using screens after lights out, and losing out on vital hours of sleep that help them develop in a healthy manner. Ensure your kids aren’t subbing screens for sleep by banning phones and tablets from bedrooms.
- Have a screen drop-off point. Put a box or basket at your front door and have family members (and friends and relatives, too) drop off technology as they enter the house. In our changing world, kids sometimes truly do need phones to stay safe, keep in contact with parents, or coordinate transportation when outside of the home. But they simply don’t need a phone on them while at home.
- Set an example. Teens aren’t the only people whose mental health is affected by screens and social media — adults struggle with phone addiction, sleep issues, and depression, too. Model the behavior you want in your kids by limiting your own screen time (you’ll also benefit!)
There are a number of helpful apps that can also help you and your kids limit screen time. While you shouldn’t rely on apps alone to restrict your kids’ engagement with technology, they can be extremely helpful tools:
- Google Family Link. This software allows you to track your kids’ activities, set time limits, and even set a bedtime — which is so important to keeping your kids healthy. Only available for Android phones and devices.
- Apple Parental Controls. These new controls work much like Google’s family controls: you can block certain apps and websites, track activity, and shut down devices at dinner time and bedtime. It also lets you see their notifications and control in-app purchases.
- OurPact. This app allows you to block websites, block apps, limit screen time, and track your child’s location. You can also schedule approved screen time and get alerts when your child leaves certain zones.
- Azoomee. This suite of hand-picked content ensures that when your kid is watching a screen, they are learning and engaged, whether they’re playing a game or watching videos. Because managing what kind of screen time your kid gets is just as important as limiting the time.
Always Be On The Lookout For Signs Of Depression
With teen depression on the rise, it’s more important than ever to be aware of the signs and symptoms of depression in your kids, no matter how much or little screen time they’re getting.
If your teen is showing the following depressive symptoms, get in touch with their pediatrician today.
- Increased crying and sadness
- Loss of interest in activities
- Insomnia or oversleeping
- Changes in appetite
- Changes in behavior, such as aggressive, disruptive, or risky behavior
- Agitation and restlessness
- Use of drugs and alcohol
- Neglected appearance and hygiene
- Poor performance in school
Having a teen can be challenging, especially in a quickly-changing world that is so different from the time when we grew up. Being aware of technology’s effects on the wellbeing of your children, as well as the signs that your kids might be depressed, are two simple actions you can take to ensure their health and happiness.
Additional Resources
- The Effect of Technology on Face-to-Face Communication
- Facebook Use Predicts Declines in Subjective Well-Being in Young Adults
- The association between social media use and sleep disturbance among young adults
- Generation M2: Media in the Lives of 8- to 18-Year-Olds
- Increases in Depressive Symptoms, Suicide-Related Outcomes, and Suicide Rates Among U.S. Adolescents After 2010 and Links to Increased New Media Screen Time
Mental Illness Awareness Week: 7 Mental Health Tips
Mental health conditions are common, and can affect anyone, young and old.
- Mental illness affects millions of Americans—1 in 5 adults (18.5%) experience mental illness in any given year. Even if not directly affected, we all know someone who has experienced mental illness.
- Despite the fact that mental illness affects so many people, lack of awareness, and misunderstandings persist.
- Mental Illness Awareness Week happens during the first week of October. Initiated in 1990 by NAMI, the National Alliance for Mental Illness, this annual event aims to raise awareness around the reality of living with a mental health condition, to provide support for those affected, and to challenge the stigma that surrounds a mental illness diagnosis.
- Mental illness affects young adults and children, too. 21.4% of those between the ages of 13 and 18 experience a serious mental disorder at some point during their lives. For those aged 8-15, the figure is around 13%. Approximately 50% of all chronic mental illness begins by age 14. Increasingly, effective treatments are now available, but long delays persist between the onset of mental health problems and seeking help. Suicide is the 2nd leading cause of death for those aged 15-24.
At Jumo Health, we are committed to raising awareness around mental illness. We see this as a critical step towards stopping the stigma that so often accompanies the diagnosis of a mental health condition. In May 2018, we launched our pledge to continue the conversation around mental health awareness. This commitment extends beyond this week, this month, to include every day of every year.
A Personal Story of Mental Illness
Jumo Health understands that personal stories- of hope, of perseverance, of strength- often carry an authentic purview that an evidence-based piece lacks. Our In My Words podcast series is one such example.
- Our mental health episodes include Gianna’s story (above) as she shares—aged 16—her experience of depression and anxiety. During her freshman year, she started to feel increasingly sad, lethargic, and reluctant to engage with her family and friends. Those close to her struggled to understand what was going on, and felt uncomfortable talking about it.
- Gianna talks about the pressure she felt as a teenager to achieve, to perform well academically, to succeed, pressures that escalated and escalated, culminating in a suicide attempt. Knowing that she could not deal with her depression on her own, she reached out for help and began her journey to recovery.
7 Mental Health Tips in 7 Days
Mental wellbeing needs just as much attention as our physical health—this applies to all of us, whether we are living with a specific mental health condition, or variously struggling with the challenges of everyday living. Maintaining mental health requires paying attention to the needs of others in addition to our own wellbeing.
- Showing your emotions is not a weakness—don’t suppress your feelings
- Admitting you need help is a strength
- Dealing with difficult emotions – remember the word PATH:
- Pause
- Acknowledge
- Think
- Help
- If you notice a friend whose mood has changed, seems to be losing interest in everyday things, reach out. You have a role—to be there without judgement or criticism, and to listen. You can make a difference. Helping others can also help you. Research has shown that teens—particularly those with social and emotional distress—who help others benefit themselves, too.
- Take care of your body. Regular exercise has been shown to improve mood and decrease anxiety and depression. Similarly, those who eat healthily tend to be happier. On the other hand, smoking and alcohol can make mental illness worse.
- Sleep well. Mental health conditions can be worsened by lack of sleep. Although it is different for everyone, it is recommended that adults should have about 7 hours of sleep per night, and adolescents, 9. Anxiety can make sleep difficult. Yoga and meditation may help the symptoms of anxiety and depression, which in turns allows for an improved sleeping routine.
- Even though mental illness affects so many people, stigma remains. We can change this by promoting awareness, and by continuing to educate ourselves on mental health, mental illness, and the experience of those living with these conditions. Get involved! There are many events throughout the year where we can show support and help stop the stigma.
Mental Health Resources
- Developing mental health resources is a top priority for Jumo Health. Check out our online store and blog posts about:
- Other resources:
- https://bringchange2mind.org/
- https://www.jedfoundation.org/
- https://www.nami.org/
- https://afsp.org/our-work/education/talk-saves-lives-introduction-suicide-prevention/
- https://childmind.org/
- http://www.mentalhealthamerica.net/
- https://theconversation.com/6-questions-you-can-ask-a-loved-one-to-help-screen-for-suicide-risk-102026
Our ability to provide a platform by which individuals can share their stories is what builds community and distinguishes it from a website. I am reminded of a quote from our blog post to mark suicide prevention month; the quote is from a colleague who chose this platform to tell her story and whose words underscore the importance of personal storytelling:
“There is hope. There is help. Some may need the help of medication…a therapist…a friend. Take one day at a time. One moment at a time. Cry when you need to. Scream if you can. Have someone listen. Listen to someone.”
Join us on Facebook, Twitter, or Instagram this Mental Health Awareness week and continue the conversation to #StopTheStigma and #OwnYourMentalHealth.
Cry When You Need To
The clattering of dinner plates. The bustling of waiters. The chatter of teenagers, celebrating the final run of their high school musical. She sits among them as the laughter surrounding her turns into a dull hum. The festivity in her periphery blurs as her vision narrows. The sinking feeling inside. She would trade this pain for any physical pain.
She blinks and the crowd is gathered outside on the cold cement. The broken street lamp flickers behind her. The roar of the racing cars ahead echoes inside her head. She stares at the headlights dancing in the darkness on Highway 17. They seem to beckon her, as she starts to walk toward them. Her pace quickens. Gaze intensifies.
A voice breaks her trance, “Hey! Where are you going?” A hand grasps her shoulder and spins her around. She collapses into her best friend’s arms, mascara running down her tear-streaked face.
Nineteen years later, that girl still doesn’t know she saved my life.
I was plagued with 4 more years of darkness following that night, until one day, the heavy curtain suddenly lifted, and I awakened to see my life waiting in front of me. I’ve since faced what seems to be an avalanche of challenges, and have feared falling back to that horrid place. But that time in my life has made me stronger. More hopeful.
Everyone has their own inner battles. I share this personal experience to let you know that, although it may not seem possible now, you will get through yours. There is hope. There is help. Some may need the help of medication…a therapist…a friend. Take one day at a time. One moment at a time. Cry when you need to. Scream if you can. Have someone listen. Listen to someone.
Additional Resources
- Our Mental Health Resource Center
- Podcast Interview with Gianna
- 6 Questions You Can Ask a Loved One to Help Screen for Suicide Risk
Asthma and Back To School: Six Steps To A Healthy Year
Back to school means new notebooks and freshly-sharpened pencils, bright yellow buses and meeting new friends. But for seven million kids in the United States alone, back to school also means worrying about asthma attacks–from where there will be triggers, to what will happen if a severe attack takes place.
The best way to have the healthiest possible year–and to quiet both parent and child anxieties–is simply to prepare. We’ve outlined six simple steps to take before diving into the new school year, especially if your child is attending a new school.
Schedule a Check-Up With Your Child’s Doctor
Kids with asthma should see their doctor for a check-up at least once each year. Doing it before the school year starts can ensure that your child has all of the prescriptions they need, that everyone has their questions and concerns answered, and that all pertinent school-related medical paperwork is filled out.
Younger children may need to be coached on their inhaler technique, while children with seasonal allergies that affect their breathing may need new medications before heading off to school. Finally, children who use peak flow meters may want to have a spare to keep at school, so that their breathing ability can be monitored on campus as needed.
Write An Asthma Action Plan
The American Lung Association has a printable, one-sheet Asthma Action Plan form that compiles all of the emergency information that you need, from a description of your child’s condition, to medication plans for different levels of attacks, to emergency contact information.
Fill this form out with the assistance of your doctor, and make enough copies so that you can distribute it to important school personnel. Alternately, your school or doctor may have similar forms to use.
Also be sure to review this form with your child–and give them an opportunity to ask questions.
Talk to Teachers and Other Important School Personnel
Meeting with the people who will be caring for your child at school is vital to their health and wellbeing. Talk to your child’s nurse or teacher–and don’t forget caregivers who might be in contact with your child throughout the entire day. This list could include:
- Your child’s teacher(s)
- Gym teachers
- Lunch and recess teachers
- After-school sports coaches
- The school nurse
- School bus drivers
- After school caregivers
Make sure each person receives an Asthma Action Plan, that they are familiar with common triggers, and that they understand the severity of your child’s condition.
Also be sure to ask the nurse about the school’s asthma-related policies and medical emergency procedures–and share any age-appropriate information with your child.
Look for Asthma Triggers at School
If your child is starting a new school altogether, request a tour before the first bell of the year rings. This can often be coordinated with meeting your child’s teacher or the school’s nurse. During the tour, ask questions about the school’s medication policies and get a clear picture of where your child will be spending their days, from their classrooms to the cafeteria. Also look for potential triggers, which could include:
- Dust and dust mites
- Chalk dust
- Mold
- Cockroach allergens
- Allergens
- Air pollution
Don’t forget to get a clear idea of when exercise could be a trigger, including recess, gym class, and after-school sports and activities–and talk to teachers and coaches about what it’s like for kids to have asthma and be active.
Get Your Asthma Medication Organized and Labeled
After you are familiar with the school’s medication policies, prepare any medication that your child will need carefully. Make sure it is labeled, has dosage information, has administration information, and your child’s name. Check everything for expiration dates, and note those in your records. Once you understand where the medication will be kept, and which medications can be kept with your child, share that information with your child, too.
Talk to Your Child–and Listen to What They Have to Say
No matter the age of your child, it’s important to talk to them about their health-related concerns about returning to school and answer any questions they might have. Remember that asthma is intricately connected to stress and anxiety–and each can act upon the other. Making sure that your child is comfortable and informed is just as important as having all of their medications and emergency plans in place.
Need more resources about asthma, for the whole family? At Jumo, we are dedicated to educate families–including kids of all ages–about their health. Check out our asthma comic book, available in English and Spanish.
References
- American Academy of Allergy Asthma & Immunology. (2018) “Back to School With Allergies and Asthma.” https://www.aaaai.org/conditions-and-treatments/library/asthma-library/back-to-school-with-allergies-and-asthma
- American Lung Association. (2018) “Back-To-School With Asthma Preparation Checklist.”http://www.lung.org/assets/documents/asthma/back-to-school-with-asthma-2018.pdf
- Centers for Disease Control and Prevention (CDC). (2012) “You Can Control Your Asthma.” https://www.cdc.gov/asthma/pdfs/asthma_brochure.pdf
- O’Brien, Sarah. (2016) “Asthma Statistics.” https://asthma.net/basics/statistics/
Why Comic Books?
I have always loved comics. As a child, I read several a week. The realisation that growing up meant moving beyond books with cartoons and panels and onto chapter books was a sad day.
Fully grown up, having left the world of comic books far behind, I studied medicine.
During my clinical practice over many years, I increasingly came to realise that too often there exists a gap between the language of those affected by illness, and the language of medicine. I started to explore this – the language of illness – more closely. Through these studies, I re-engaged with the world of comics, which by this time had started to emerge as a distinct genre within the world of literature. The era of the graphic novel had arrived. Graphic novels and comic books are pretty much the same thing – graphic novels are sometimes described as comic books with chapters.
With colleagues in medicine as well as the humanities, I was involved in the first Comics and Medicine conference, which was held in London in 2010. This is now an annual event, alternating between Europe and the US.
The visual / verbal format is well positioned for relaying information as well as the emotional components that inevitably accompany illness. There are many reasons why comic books facilitate the communication of difficult and complex medical information, including:
- Efficient use of text. Comic books contain less text than their non visual counterparts, which means that the words used are chosen deliberately.
- Words and images complement each other. Thus, for the reader who might not fully understand the text explanation, the accompanying visual serves to clarify. This makes the format particularly useful for complex medical topics.
- The format appeals to different audiences – it pulls in readers who prefer visuals as well as those who respond better to words.
- The visual component allows a showing of emotions, rather than merely describing them with words.
Comics have been shown to enhance learning within the classroom. In one study, students read either the traditional text of Shakespeare’s Hamlet’s or a graphic novel version. Those who studied the graphic novel spent about an hour less reading and scored higher on a comprehension quiz.
The potential value of comics to relay health information has also been studied. This review demonstrated the potential of comic books in the health field to enhance self-awareness, reassurance, empathy, companionship, in addition to their strength as a means of exploring the impact of illness on family relationships. The author concluded that comics are under-utilised in terms of their potential to enhance understanding and to deliver support in this context.
Within the health care setting, comics have many potential educational uses – patient support and care, patient education, education for medical students and healthcare workers, caregiver support, healthcare community programs.
Graphic medicine – the use of comic books in the area of medical education and patient care – has now become a field in itself. Check out this great website that features reviews of very many graphic novels and comic books, all related to health and illness. It was originated by Ian Williams, MD, in 2007, with the following goals:
- Reflecting or changing cultural perceptions of medicine
- Relating the subjective patient/carer/provider experience
- Enabling discussion of difficult subjects
- Helping other sufferers or carers
Here at Jumo Health, we use the comic book format to help educate and support children and their families affected by illness. Our content features real children, and their stories, which enhances the relatability of their experience to their peers. Understanding what is going on when you have a chronic medical condition is not easy, and as a result it can be very difficult for children and young adults to share their stories with others. The comic book format, the graphic representation of what living with a specific illness both physically and psychologically really means, facilitates not only an understanding of what is happening in the body, but also helps those affected feel less isolated as, through knowledge, they gain confidence about sharing their experience.
Comic books, with their dynamic visual action stories that work around information on health and illness, uniquely allow for this.
Today, September 25, is National Comic Book Day, a very special day here at Jumo Health. Check out our digital comic books, audiobooks, podcasts and more.